What Yoga Trains that Metrics Miss
by Karen Kraft Rigsby
A New Year and a new (perhaps) perspective on yoga. I would like to thank Karen Kraft Rigsby for accepting my invitation to share her incredibly valuable experience with yoga, both academic and interoceptive. As someone who largely rejected yoga for years, I will be the first to admit that its practice, her practice, has changed the way I approach physical therapy, coaching and cycling. I am going to lead with a few accolades, which she is too humble to share.
Drafter handle is “Pipes”.
Olympedia: Karen Kraft rowed the pair at the 1996 and 2000 Olympics, winning a silver medal in 1996 and a bronze medal in 2000. She also competed in the pair at the 1995 World Championships and the 1999 Pan American Games, winning silver medals at both regattas. At the Lucerne International Regatta she won a gold in the pair in 1996 and a bronze in 1995.
Kraft rowed in college at Cal Poly, San Luis Obispo, although it was only a club program. She later became a rowing coach at the University of Wisconsin. Married and later Karen Rigsby, she also works as a yoga teacher and personal trainer.
United States Postal Service First Day of Issue Women’s Rowing May 13, 2022 featuring Karen Kraft Rigsby
The Side Door
I came to yoga through the side door of science, after my rowing career ended. I was in graduate school at UW Madison, studying exercise physiology—curious about efficiency, adaptation, and performance. Yoga began as an academic exercise: a way to study range of motion, breath mechanics, and nervous system regulation. Maybe, I hoped, it would also ease some of the chronic wear and tear that came from spending a decade in the sport of rowing which—much like cycling— lives largely in the sagittal plane.
Yoga didn’t stay academic for long.
It didn’t just change how my body moved; it changed how I experienced effort. It taught me how to stay present instead of disappearing into repetition or the familiar refrain that “harder is always better.” Or “hardest is best.” It taught me to listen before pushing. To remain steady when sensation got loud.
I never practiced yoga during my Olympic quadrennials. I often wonder what would have been different if I had. In 1996, three-tenths of a second separated my silver from Aussie gold. I believe—without hesitation—that yoga would have erased and reversed that margin. Not because I would have been stronger, but because I would have been clearer. Calmer. More available in the chaos.
But more than the medal, it would have changed the seven minutes before the finish. It would have shaped the years of practices leading to the Trials. It would have altered how I lived alongside the training itself. I may have come to yoga for performance—but its real gifts aren’t measured there. They’re found in the life that unfolds alongside effort. Even those two Olympic berths would have been lived differently.
If yoga had been part of my life then, the race itself would have unfolded more fully in flow—that rare state where time loosens and the mind goes quiet. I don’t think I would have remembered much of it. As it is, I remember plenty: the moments when my mind started whispering its small, unhelpful stories. With yoga, more of that race would have lived in the body’s knowing rather than the mind’s commentary. And a gold medal would rest quietly in a sock drawer, instead of a silver and a bronze. Indubitably. But enough about me.
A Different Kind of Adaptation
Yoga is not a “check-all-the-boxes” panacea for a fitness program. It isn’t about calories burned, heart-rate zones, or maximizing muscular output. Those frameworks belong to conditioning models built around external metrics. Yoga operates differently.
At its core, yoga is a wellness practice—a movement ritual and an awareness tool. It develops interoception (our ability to sense what’s happening inside the body), postural integrity, neuromuscular coordination, and attentional control. The adaptations are subtle but profound: improved joint recruitment, expanded range of motion, refined motor control, and a nervous system that learns how to regulate rather than react. For more on the studied (not just postulated, unproven) benefits of yoga, this article is robust.
Hot yoga, in particular, has often been marketed as a high-intensity cardiovascular workout. From a physiological standpoint, that framing misses the mark. Elevated ambient temperature does not increase oxygen demand in skeletal muscle nor does it drive mitochondrial ATP production beyond normal exercise requirements. Sweating is simply a thermoregulatory response—evaporation cools the skin and helps maintain core temperature. It is not a proxy for effort, fitness, or energy expenditure.
The heated yoga styles, to a point, can increase tissue pliability, support fascial and connective-tissue mobility, challenge proprioceptive focus, and promote heat acclimatization. A hot yoga practice also demands greater attentional regulation from the central nervous system. But dripping sweat is simply evidence of thermoregulation at work—not a reliable marker of maximal training stimulus or cardiovascular demand.
Yoga’s value lies elsewhere: in resilience without impact, coordination without force, and awareness without overload. This perspective is echoed in an article by a former yoga teacher turned PhD in exercise physiology, who describes intentionally “disentangling” yoga from the idea that it serves as a panacea for all forms of physical training.
Stillness Has Always Been the Point
Yoga did not begin as a physical fitness practice.
Its roots stretch back 3,000–5,000 years to ancient India, where yoga functioned as a spiritual technology—a system for quieting the mind, reducing perceived suffering, discerning truth, and loosening attachment to compulsive patterns of thought and identity. Postures existed, but only in service of a single aim: to make the body stable and comfortable enough to sit, breathe, and pay attention during long hours of meditation.
In short, yoga was “invented” so monks could remain seated in stillness for hours at a time.
It was inward. Disciplined. Often austere. Yoga was centered on breath regulation, ethical living, concentration, meditation, and clarity—not performance, productivity, or fitness.
Modern yoga emerged much later, in the late 19th and early 20th centuries, as Indian teachers responded to colonialism, reclaimed physical vitality, and translated ancient practices for changing bodies and cultures. Standing poses, flowing sequences, and strength-based postures made yoga more embodied and accessible.
This wasn’t a corruption of yoga, in my opinion. It was a translation. And yes, some things were lost in the translation…as they almost always are. But, the heart of yoga didn’t change - just the doorway. The problem that yoga was designed to solve hasn’t changed—only the setting has.
Why The Old Intelligence Still Applies
Many sports live in a narrow lane of movement. Cycling, for example, occurs largely in the sagittal plane—forward moving—requiring the rider to remain seated for long stretches while generating power through the pedals. Success isn’t just about force production; it demands balance, stability, and sustained attention while the world moves beneath you.
Rowing shares this intelligence. The athlete remains seated, moving forward and backward within the shell, stabilizing through the core as the boat slides through the water. Each stroke adds subtle rotation to catch the water with the oar and propel the boat efficiently. Both sports are repetitive, powerful, precise—and also narrow, with movements repeated thousands of times.
This is where yoga’s legacy becomes unexpectedly relevant. Long before it was a movement practice, yoga existed to prepare the body to remain seated for hours of meditation - with steadiness and clarity—to regulate breath, sustain focus, and quiet reactivity over time. On the bike, the object of attention isn’t a scriptural text but cadence, terrain, and breath. Add wheels, speed, and subtle instability, and the ancient skill still applies: staying present, steady, and responsive while motion unfolds.
Yoga widens the lane. It asks the body to rotate, side-bend, extend, stabilize, and release—to move fully and often in all directions. And when the body moves the way it’s meant to move, the brain and body stay in conversation. They don’t separate into autopilot or pure “muscle memory.” Presence stays online.
Ironically, this awareness is what allows flow—the effortless, responsive state athletes recognize when mind, body, and breath align. In sport, flow can mean smoother technique, steadier pacing, and sharper timing. Yet flow is not the goal; it emerges from sustained attention and adaptability. By moving in novel ways, linking breath with motion, and holding awareness through subtle challenges, yoga trains the brain’s attentional and sensorimotor networks—the very mental agility athletes rely on to step into flow.
Yoga doesn’t exist to fix the body or make athletes more flexible. It exists to interrupt patterns, expand awareness, and teach the nervous system to respond rather than react. When the body moves differently, the mind often follows. Perspective widens, and the nervous system absorbs new information.
Yoga can also be seen as stress inoculation: the body is intentionally placed in mildly challenging positions—unfamiliar shapes held for several slow, deliberate breaths. Sensation rises, but the context remains safe, allowing the nervous system to experience stress without being overwhelmed. In that space, something important happens. The sympathetic response may rise, but it is met—almost immediately—by steadiness: breath, attention, choice. Instead of escalating into fight or flight, the system learns to stay. To listen. To respond rather than react. Over time, this trains autonomic regulation, teaching the body that intensity does not automatically require urgency.
These small, repeated exposures build resilience. Much like a vaccine, yoga offers a measured dose of stress that allows the system to adapt. When pressure shows up off the mat—during training, competition, or daily life—the nervous system recognizes the pattern and finds its footing more quickly.
And the dose doesn’t need to be extreme. Yoga doesn’t require ninety minutes in a 105 degree room. It can be practiced in short, intentional intervals: fifteen or twenty minutes of mindful movement, or even a single awkward shape paired with unfamiliar breaths. Sometimes all it takes is a brief interruption in the body’s usual rhythm to loosen the mind’s habitual grooves—and make space for steadiness, clarity, and choice.
Yoga functions as an awareness practice. As we balance in unfamiliar ways, breathe under mild stress, and move outside habitual grooves, we begin to notice how easily our thoughts and emotions fall into ruts of their own. Whether you call that clarity, regulation, flow, or something more sacred doesn’t really matter.
What matters is that yoga creates space.
Space to notice.
Space to choose.
Space to respond rather than repeat.
Yoga Styles — A Practical Lens
Movement & Flow
Vinyasa / Flow — Breath-linked sequences building strength, coordination, and awareness in motion.
Ashtanga — A fixed, demanding series emphasizing discipline, stability, and breath under load.
Hatha — Slower, foundational postures developing joint awareness, alignment, and controlled transitions.
Alignment & Tissue Health
Iyengar — Precision-based practice using props to optimize joint mechanics and postural balance.
Yin — Long-held, low-load postures targeting connective tissue and joint hydration.
Restorative — Fully supported poses that downshift the nervous system and support recovery.
Mind & Regulation
Kundalini — Integrates breath, movement, and meditation to support focus, emotional regulation, and stress resilience.
As one of my UW student-athletes put it, capturing both the surprise and the simplicity of a beginner’s journey:
“I never realized how disintegrated I was. Yoga has shown me the power of bringing my mind into my body instead of placing it on top of it. My performance on the track has changed—my coach has noticed. I really think it’s the yoga. Who knew?”
Sometimes the most meaningful gains don’t come from pushing harder, but from arriving—fully, quietly, and on speaking (and listening) terms with yourself—where each twist, turn, and tilt off the familiar lane widens the scope of how you feel, move, and live.
TRAIN WITH KAREN
Yoga practice should be what you need it to be. For me, and most of my athletes, finding a class that speaks to you and fits your schedule can be a barrier. For these reasons, I have asked Karen to create a series of ~ 30 minute mini-yoga sessions specifically for the time crunched cyclist, or anyone who is bound by the sagittal plane.
🧘♀️ Session 1 Hip and Thoracic Spine Mobility
🧘♀️ Session 2 Shoulder and Thoracic Spine Mobility
🧘♀️ Session 3 Hip and Core Strength
🧘♀️ Package: All 3 Videos + Bonus Strength Video
These classes can be purchased individually for $75, or as a package for $200. The package purchase includes a bonus fourth session with strength challenges (7 min). Click the links above to purchase your session(s). You will receive an email within 24 hours with a private link to access these videos on YouTube.
Happy New Year.
Draft responsibly,
BrickO
Winter In and Out
The forecast for the weekend is promising snow. Lots of snow. Are you ready?
Snow and cold don’t have to be miserable. With the right equipment and attitude, winter months can be an excellent opportunity to change up and charge up your training stimulus.
I think there are two broad categories of Wisconsinites: those who embrace the cold and continue to find joy training in it, and those who don’t. No judgement, just don’t waste time fooling yourself. Get busy making the best of whichever camp you are in.
For those who enjoy the great white, snow provides a rich cross-training opportunity. Cross country skiers have the largest aerobic engines (highest VO2max- see records below). In part, it requires full-body muscular engagement. It is low-impact, but not quite as low as cycling, and your butt gets a break from the saddle! Classic XC (diagonal skiing) has a similar neuromuscular pattern to cycling, engaging glutes, hamstrings and quadriceps in the sagittal plane. Like cycling, XC skiing requires smooth force activation to maintain economical motion and builds a huge aerobic base with minimal risk of overuse injury.
Drafting responsibly
4 of the 6 world record holders for VO2max belong to cross-country skiers.
MALE
96.7 ml/kg/min | Oskar Svendsen
In August of 2012, Svedsen tested the highest VO2 Max measurement in recorded history before the 2012 Junior World Time Trial Championships.
96.0 ml/kg/min | Bjørn Dæhlie
Dæhlie is well-known for his career in cross-country skiing. He won the Nordic Cup six times and won a total of 29 medals in the Olympics and World Championships between 1991 and 1999, making him the most successful male cross-country skier in history.
96.0 ml/kg/min | Espen Harald Bjerke
Norwegian cross-country skier, tested at 96 ml/kg/min in 2005.
FEMALE
78.6 ml/kg/min | Joan Benoit
The first women’s Olympic Games marathon champion, winning the Gold medal at the 1984 Summer Olympics in Las Angeles.
76.6 ml/kg/min | Bente Skari
Hailing from Norway, Skari is one of the most successful cross-country skiers ever, receiving 12 Olympic and World Championship medals.
76.0 ml/kg/min | Flavia Oliveira
A Brazilian racing cyclist who finished in 7th place in the 2016 Olympic Games in Rio de Janeiro.
More than just 3 good looking VO2s
Skate XC skiing changes things up a bit, with more demand on balance and stability due to the rapid weight shift. Powerful movements in the frontal plane recruit muscles that are largely ignored during cycling. While both types of XC skiing can incorporate intervals for threshold and VO2max, most turn to skate skiing for this stimulus due to the high demand for power production.
For the pure cyclist, there is still riding to be enjoyed in the snow. As much as I love XC skiing, I haven’t put on sticks since purchasing a fat bike. Of all the cycling modalities I enjoy (road, gravel, MTB), fat biking is far and away my favorite. It is hard to describe the feeling of riding through the woods, trees offering protection from the howling winds, their branches heavy under a blanket of snow, rays of the sun (maybe) catching the falling flakes, throwing prisms of light that dance at your feet. The only sound is your breath, echoing inside your insulated helmet, ski googles and face mask. For me, it is nirvana on a bike.
Drift Drafters at the Fat Tire Birkie
Weather patterns are changing, leaving snow less of a certainly in the winter. While this is a disaster for skiing, frozen lakes void of snow provide miles upon miles of unadulterated fat fun. Stud up your tires and away you go!
A day on the lake
Liberty and Fat Bikes for All
There are plenty of fat bike events to test your mettle and your metal.
Fat Tire Birkie, Hugh Jass Series, Snow Crown Series, Tuscobia Winter Ultra to name a few.
There are lots of reasons why XC skiing and fat biking may not appeal to you: cost of gear, limited daylight to train, or aversion to the cold. In that case, winter is a great time to build your base on the trainer. For some cyclists, the trainer is a godsend. It is incredibly efficient and a guilt free ticket to binge watch Stranger Things.
If you are interested in riding with some familiar faces, consider this GREEN FRIDAY deal for Drafters only to join Source Endurance training through Velocity. This is a Zoom meets Zwift platform developed by former professional, Robbie Ventura to help coaches build community with their riders.
I’ll be leading two rides each week for Source Endurance, Wednesday and Friday 7-8AM for 12 weeks, Dec 3, 2025- Feb 20, 2026. Enjoy a 2 week free trial, and then decide if this is right for you. Drafters receive a 25% discount!
You’ll need a trainer and a laptop/tablet/phone with the Velocity app. Power is not required- you can use HR or RPE to stay in the zone. You will see other riders in the class, and their power and HR gauges (see image below) but their actual numbers will NOT be visible. If you are hitting the right zone and cadence, your gauges will light up green, over the target will illuminate red and under will light up blue.
Can’t make W/F 7AM but still interested? No problem. The classes will be recorded so you can replay it at any time, as many times as you’d like. The recorded class will also be replayed the following T/Th at 7AM so if you join, others may also be there “live”. Robbie has also generously agreed to provide a dozen or so of his favorite workouts.
COST: $100/mo. Green Friday discount code for Drafters only: 25%. This will knock the cost down to $75/mo, or ~$10 per class, and includes to Velocity app fee ($20/mo).
Click here to sign up for your two week free trial. If you aren’t enjoying the platform (or me) after the free trial, no hard feelings. I appreciate you giving it a try.
Oh what fun it is to ride
A few cautionary pointers for indoor training:
The trainer is stationary. Obvious, and yet cyclists often rock their body over the bike to get the leverage. These are not the same force vectors through your joints as rocking the bike underneath your body. I’d caution against it.
Air flow. Unless you are racing in AZ in February and working to heat acclimate while in your cycling studio, be sure to have a fan and maybe crack a window. Sweat on the floor = waste of evaporative heat potential.
Hydrate and fuel as you would outside. Gut training can start now for your ultra event next season.
Bike fit. Many cyclists have an old bike and shoes relegated to the trainer. Be sure the old bike has your current bike fit. If the saddle is different, consider swapping for your current saddle. And check your cleats. Worn cleats = knee pain.
I hope to see you drafting responsibly, in the snow or on the trainer.
BrickO
The Weight Room is Calling
Winter is coming. The best place to weather the storm may be in the weight room.
The off-season is an opportune time to build or rebuild strength. Strength is the amount of force that can be produced and transferred to push (a pedal) or pull an object. Over the course of the cycling season and without maintenance weight training, strength can decline up to 25%. While your functional threshold power may be going up, it is likely due to improved muscular metabolic machinery (mitochondria) and cardiovascular adaptations, and not to strength gains.
Pedaling your bike, even up steep hills, does not provide ample stimulus to build strength. The load per pedal stroke may feel “hard”, but given that it may be repeated thousands of times during a ride, it does not reach the critical threshold to build strength. Furthermore, heavy endurance training load, which can lead to glycogen depletion, both suppress the signal for increased strength.
The off-season allows time to rebuild the machine! Strength gains can be achieved through hardware and software upgrades. Some theorize that hardware (big muscles) is for show and software is for go.
To understand the roll of strength training on upgrading the hardware, let’s talk about some of the proteins involved. Figure A below depicts how the muscle fiber contractile proteins, myosin and actin, are organized within Z lines to produce a functional unit, called a sarcomere. Figure B is a brilliant illustration to demonstrate how myosin hands (called heads) grab onto actin (forming a cross bridge). It is easy to imagine myosin hands pulling actin towards the midline to shorten the distance between the Z bands (sarcomere).
The Sliding Filament Theory of Muscle Contraction
By: Jacob L. Krans, Ph.D. (Dept. of Biology, Central Connecticut State University) © 2010 Nature Education
Citation: Krans, J. L. (2010) The Sliding Filament Theory of Muscle Contraction. Nature Education 3(9):66
Strength training hardware upgrades occur through protein synthesis of actin and myosin to increase the cross-sectional area of the muscle (hypertrophy). Simply stated, there are more hands to do the work. Hypertrophy occurs in all fibers (slow and fast twitch); however, fast twitch fibers have a greater potential for growth. This works out well, since fast twitch are also the first to atrophy (lose cross-sectional area) during the cycling season.
Strength gains are also made through upgrades in software, represented by our central nervous system (CNS). These are the gains seen initially in the first several weeks of weight training. In order to understand the software upgrades, let’s quickly touch upon two ways in which force can be increased.
Strength training can increase force through the following software (signal) upgrades:
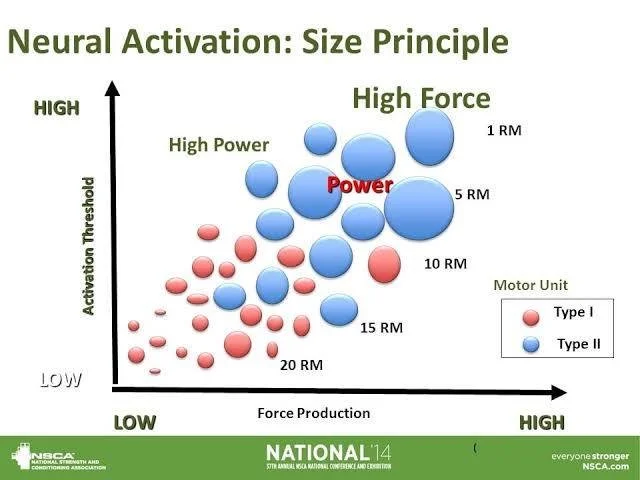
1. Recruitment. A motor unit is defined as a motor neuron and all the muscle fibers it innervates. When the brain sends a signal to a motor neuron to contract a muscle, all of the fibers in that motor unit are activated. This is referred to as the all-or-none principle. Realize that NOT all motor units in a given muscle are recruited for sub-maximal efforts, only ALL the fibers within a motor unit. This gives us the ability to grade our force. Recruitment of motor units is based on Henneman’s size principle, which states motors units are recruited from smallest to largest. Size refers to two things: 1) the size of the motor neuron cell body, and 2) the number of fibers in the motor unit. Neurons with small cell bodies innervate slow twitch fibers, typically 10-200 fibers per motor unit. Neurons with larger cell bodies innervate fast twitch fibers, typically 500-2000 fibers per motor unit. Fast twitch fibers produce more force but are less efficient than slow twitch.
Strength training increases the ability to recruit more motor units for a stronger contraction through greater neural drive. Strength training also improves synchronization of recruitment so there is less division in the timing of recruiting slow twitch (Type I) and fast twitch (Type II) fibers. Cyclists benefit from increased neural drive and synchronization of recruitment for sprint acceleration, improved ability to snap out of corners and surge to attack.
2. Increased firing rate (summation of twitches). A nerve impulse (twitch) will signal all the fibers in that motor unit to contract. When the firing rate is slow, the muscle fibers generate low force. This has to do with calcium transients. As the twitch rate increases, the force increases as the cross-bridges do not have time to relax (more calcium hanging around). With rapid firing rate, maximal force is reached (calcium has allowed more cross-bridges to form within the fiber). This is another way in which we grade force. Strength training increases the software to deliver more rapid firing, which gives a cyclist more force per contraction as more cross-bridges per fiber are formed.
How do I upgrade my hardware and software?
Acquiring more hardware is achieved by lifting lighter weights with greater repetitions to create a stimulus for hypertrophy (muscle cross-sectional area). Increasing strength through software upgrades (central nervous system) can be achieved through lifting heavier weights and fewer repetitions, creating greater muscle fiber recruitment. The balance between these basic types of lifting prescriptions changes based on: 1) athletic age of the athlete (how long have they been strength training), 2) injuries or imbalances, 3) phase (off-season, base, build, peak, maintenance), 4) type of lift (primary, secondary, accessory) and 5) goal of strengthening.
This is where I find working with a Certified Strength and Conditioning Coach to be really helpful. Please visit the Community Partners page for information on Drafter Strength Training classes at Digman Fitness. Plans are easy to find on line, but the one that is right for you likely requires a more personalized approach.
Phases of strength training mirror the periodized phases of training on the bike with transition/off season, phase, base, building, peak/race. All phases of strength training involve primary, secondary and accessory lifts.
Primary lifts include multi-joint and larger muscle groups. These compound lifts require the most coordination, and therefore place the biggest load on the neural system (software). Examples include squat (front and back), Romanian dead lift (RDL) and lunge/split squat. Examples of push and pull compound lifts for the upper body include bench press and rows. In general, primary lifts will be done at a higher percent of one rep max (%1RM) with less reps and more sets compared to secondary lifts (roughly the same total number of lifts).
Secondary lifts reinforce those movement patterns, but are done with slightly lower load and more variation in stance, for example single leg or split stance. Examples include Bulgarian split squat (BSS), step-up or step-downs, hip thrusts, Nordic hamstring curls and goblet squats. Upper body secondary lifts might include dumb bell rows, bicep curls and tricep extensions.
Accessory lifts are designed for stabilization and are typically done with low load, high reps, short rest with a focus on control. Examples include glute bridges, single leg RDL, calf raises, banded monster walks, core (planks, dead bugs) and scapular stability (Y-T-W raises).
The off season or transition phase may be very dissimilar between cyclists. For the cyclist with strength as a limiter, or an athlete who has never engaged in weight training, or coming off of an injury, a block of hypertrophy focus may be recommended. The goal is to build hardware and teach proper form with moderate loads, RPE 6-7. Rest is relatively short. This will translate into a foundation from which to build strength.
Phase: Off-season/Transition
The base phase of strength training emphasizes max force and neural software upgrades through much higher loads (RPE 7-9), and therefore less reps (roughly half compared to the hypertrophy protocol), and more rest (nearly double). This will translate into increased peak torque for climbing and sprinting, and a foundation for explosive power.
Phase: Base
During the build and peak phases, explosive lifts and plyometrics are introduced. Strength training focuses on the rate of force development, or power, emphasizing the fast concentric phase rather than time under tension of the eccentric phase. Loads remain high as in the base phase, but reps and sets are reduced. This provides a stimulus for maintenance without building fatigue. Core exercise should remain a staple of all phases.
Phase: Build, Peak
During the competitive season, a maintenance phase is employed. Strength training may drop to one time per week, limited to 2 compound lifts, functional training to maintain mobility, and core. This is enough stimulus to preserve strength hardware and software.
The numbers make my head spin, but if you understand strength upgrades, and the purpose of lifting throughout the various phases of training, the reps and sets make sense. I hope. Strength coaches may have a very different approach to the general guidelines noted above. Be sure to know why you are lifting as that will guide how you are lifting.
Stay strong and lift responsibly.
Emphasis on FTP: Fun to Play
This blog post is not rooted in the pillars of movement, physiology, training measures or metrics. What has been missing from all of these informative posts is a key element to successful training: Fun. Make no mistake, not every Tabata workout or 5 x 5 VO2 interval session is intended to be fun. Not every ride is going to be a love affair with your cycling machine. There is little chance for physiological adaptations and performance enhancement when the prescription calls only for fun.
But what if one day each year, fun was the prescription? Welcome to the 4th annual Funtathalon, where Functional Threshold Power FTP in watts is leveraged against FTP numbers in Fun To Play.
Extra fun was had by the two teams in the center: Can Am with defining socks and Brazen Ballerinas with colorful matching bibs.
Each team was tasked with picking a jersey color for easy identification on the course. That backfired, as 4 teams selected blue and 2 orange. Luckily, Online Cycling Gear has 50 shades of blue. Team name selection added to the concoction of fun: Herbie & Jim Douglas, Krusen, Trout van Aert, Are We Late?, CanAm (note the socks), Brazen Ballerinas (note the bibs), Easy Beats, Bone Crushers, Where’s The Swim Start? and Tropical Thunder Biking Wonders.
Behind each team name, there is a fun story.
A key ingredient for fun is safety. This requires a large crew of volunteers, both in transition and out on the course.
The sequence of the four riding events is MTB, road, gravel, road. Each rider must compete two of the four events. Historically, teams have elected one rider for the road and the other for off road segments. Henceforth, the riders will be referred to as “roadie or dirty” Funtathletes. Logistically, this creates a natural break between segments and also minimizes the number of bikes each team has to bring. Not to be confused with the number of bikes each Funtathlete has to own, because we all know fun = N+1 rule.
Starting position for the MTB race was determined by a game of Granny Pants. Wind sprints to collect each ball and scoring 3 balls in Granny’s Pants filled the fun meter. Lessons learned: set up Granny Pants downwind, and have a curb or plenty of kids on hand to retrieve balls.
While 10 dirty Funtathletes were shredding the MTB trails, their roadie teammates were earning points playing Corn Hole. There was a delay of game when a pair of MTBers leaving the park accidentally drove over one of the boards with their pick up truck. We made it fun! All 10 teams shared one board to complete 4 tosses.
Corn Hole resulted in zero injuries, aside from one of the boards. The Brazen Ballerinas had the most finesse. The judge, a former ballerina herself, ruled with fairness, despite marital relations with a team member of Easy Beats.
As our volunteers on course started ringing cow bells from deep within the woods, the roadies readied their trusty steeds in the corral.
Transition 1: the roadies await the arrival of their dirty MTB teammates.
No aerobars or TT bikes were allowed, but Easy Beats’ roadie pulled cobwebs off of his spokes, trying to decrease his drag. The spiders have been working on his bike since the Funtathalon in 2024. Other teams have perfected this taper technique. Here is a clip of Are We Late? road racer the week before the Funtathalon. Are We Late?, Bone Crushers and Krusen are balancing professional cycling careers with full time jobs and raising 3 small kids. There may have even been a breast pump at the Funtathalon tent. Sometimes the fun is in watching your kids learning to ride rather than training to race.
It was a tight MTB race, with Love Bug’s Jim Douglas first out of the woods, followed closely by Hammer Time.
And off they go! The 20 mile road segment is mostly downhill. WHEEEEEE. That’s fun!
The race was on to beat the roadies to Transition 2. With heavy construction and the promise of the exit ramp closing, much fun was had dodging cones. No traffic laws were broken (safety first). A second wave of volunteers had T2 heavily stocked with hydration and fuel, and games!
The dirty teammates played Kubb to earn points. Toss a stick, knock down a pin, earn a point. Knock down the king pin, game over. Tropical Thunder Biking Wonders dominated Kubb, although there is no photo evidence of their feat.
Refueled and rested, the dirty Funtathletes made their way to the T2 corral. The gravel segment is 20 miles of mixed surface, roughly half gravel and grassy double track through a State Park. Everyone bought a State Park pass, because it is fun to do the right thing.
Dirty gravel Funathletes await the arrival of their roadie teammates.
Trout van Aert was the first to arrive! Go fish.
There was more fun to be had at T2! While the dirty Funtathletes were out grinding gravel, their roadie teammates were busy with monkey business. Monkey Tail is a game of precision, balance, quad strength and healthy knee cartilage. Kudos, again, to Tropical Thunder Biking Wonders on their amazing ability to swing.
After swinging their tails, the roadies high tailed it up to the transition area to await the arrival of their dirty teammate. The gravel course produced no injuries, despite a tree down on the 2.3 mile grassy double track. This was fun for the cyclocross racer of team Herbie and Jim Douglas, who bunny hopped the obstacle.
The safe return of all 10 dirty Funtathletes concluded the off-road segments of the Funtathalon.
With the final segment of the road race was underway, so were the fun shenanigans. Funtathletes were challenged with Fish Food and a shot of whiskey (NA option available), along with Trivia. 10 questions were designed to highlight something special about each of the 10 teams. Funtathletes collaborated to learn what they didn’t know about one another: Trout van Aert is getting married, what type of band are they having? Bone Crushers just added a junior Drafter to their family, what’s his name? CanAm is the only team to have competed in all 4 Funtathalons, what was their previous team name?
The 23 mile road segment included the most fun the Driftless has to offer. Living up to the rafter motto, “When in Doubt, Climb”, this route captured 1800’ of scenic elevation. In an incredible display of sportsmanship, roadies from teams Are We Late?, Bone Crushers and Easy Beats competed for the Lantern Rouge trophy.
There were awards, but I think these photos capture the real win. Volunteers and racers, grandmother and grand daughter, sisters, husbands and wives, friends. All gathered together to have fun on bikes.
On a serious note, obesity is plaguing our country. In 1970, 5% of children and 15% of adults were obese. Today, those numbers have inflated to 20% and 40%, respectively. There are a myriad of contributing factors, one being habits in youth are driven towards organized sports versus free play. According to ChatGPT (I can’t believe I just said that):
Specialization Pressure
Early specialization (e.g., year-round single-sport training) can burn kids out physically and mentally.
Dropout rates are high: by age 13, ~70% of kids quit organized sports (often because it’s no longer fun).
Once they quit, many don’t replace sports with free play—so activity levels collapse right when adolescence and lifelong habits are forming.
Fun Matters
Kids and adults are wired for play—exploration, games, variety. When activity is joyful, they choose it.
When activity feels like work (drills, performance pressure, body image), people disengage.
Research shows enjoyment is the #1 predictor of whether kids stick with physical activity into adulthood—not performance, competition, or winning.
A culture shift may be needed: from “fitness as training” to “fitness as fun” (games, movement, social play).
Fun is a key component to maintaining compliance with exercise and building community. A special thanks to all of the volunteers who helped make the Funtathalon safe and successful. And to all 20 Funtathletes who put themselves on the starting line to have fun and support one another. FTP = fun to play.
Save Your Breath
Our last two newsletters have brought us up to speed on respiratory anatomy and physiology, and using ventilatory thresholds (V1 and V2) to monitor training intensity. What if we could use breath to train AND train to have more breath?
Most cyclists are familiar with training skeletal muscles to improve pedaling performance. Squats and deadlifts may give us more power through the pedal. Could adding resistance training for our diaphragm and other inspiratory muscles provide a performance benefit? And what about those Breathe Right nasal strips worn by Team Visma | Lease a Bike in the Tour de France?
The answer to these questions is best answered by asking a different question: what is the limiting factor in maximal oxygen consumption (VO2max) and performance? If the answer is ventilation, then perhaps there is merit to exploring inspiratory muscle training (IMT) or nasal strips to improve VO2max and performance.
Before we look at the research on IMT and nasal strips, a short physiology review on ventilation as it relates to VO2max.
VO2 can be described by the Fick equation for oxygen supply and demand.
VO2= cardiac output x arterial-venous O2 difference.
This equation represents the interplay between oxygen supplied by the heart (cardiac output = heart rate x stroke volume), delivery (oxygen rich arterial blood) and utilization (tissues demand oxygen- the rest is returned to the heart in oxygen poor venous blood). During exercise, oxygenated blood to organs like the gut is shunted away and redistributed to working skeletal muscles. This redistribution is very effective in using most of the oxygen available. Very little returns in the heart in the venous blood.
In order for oxygen to be consumed by working muscles, it must pass through four stages of gas exchange. A limitation in any of these steps could impact maximal oxygen consumption.
Ventilation (airflow in/out of lungs)
Gas exchange (oxygen diffusion from lungs to blood)
Cardiac output (pumping capacity in L/min) and oxygen transport
Muscle oxygen utilization
There is little debate that the supply chain (3, cardiac output & oxygen transport) is the primary limiting factor in VO2max. Muscles demand more than what the cardiovascular system can supply, due in part to training adaptations, such as increased mitochondrial density, mitochondrial enzyme activity and capillarization (4, muscle oxygen utilization).
So that’s it, right? If cardiac output is the limiting factor, only performance enhancing strategies aimed at increasing supply, like blood doping, would be effective. Why even open up a discussion about breath training?
We noted in the anatomy and physiology newsletter that the lung is “over built” with respect to capacity. Ignoring disease states such as asthma or COPD, structural airway issues like a deviated septum, ventilation (1) is not a limiting factor.
Or is it? Here is the argument for nasal strips: breathing through the nose vs the mouth offers the benefit of air purification and humidification. At high volumes and velocities, the nasal passage is often limiting, forcing cyclists (and other athletes) to mouth breathe. If we clarify that ventilation isn’t a limiting factor, but rather ventilation through the nasal passages is limiting, then perhaps the nasal strips have merit.
Nasal strips may increase nasal cavity cross-sectional area, stabilize the nasal vestibule and increase airflow, which gives the perception of reduced dyspnea (shortness of breath). We know that the perception becomes reality, so it may very well be that these athletes feel as though can perform better. The data does not support that theory.
A 1999 cycling ergometer trial found no difference in cardiorespiratory function, work output, and perceived exertion using nasal strips vs placebo. More recently, a 2021 systematic review and meta-analysis of over 600 studies found the external nasal dilator strip showed no improvement in VO2max., HR and RPE outcomes in healthy individuals during exercise. But they sure look like fun.
There is surprising and revolutionizing data out of Jerome Dempsey’s lab at UW- Madison to suggest that in highly trained endurance athletes, gas exchange (2) may impact performance (review). Recall that the alveoli of the lung do not adapt to training, while capillarization and perfusion of the alveoli adapt well to training. This creates a mismatch between ventilation and perfusion (V:Q ratio we talked about in the anatomy and physiology newsletter). Paradoxically, the more fit and adapted an athlete becomes, the more likely gas exchange inefficiencies are to occur. This mismatch doesn’t have a solution, certainly not nasal strips.
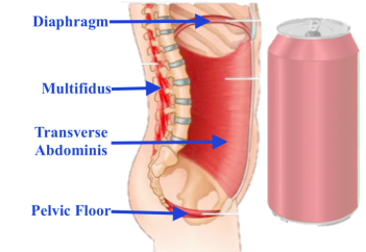
There is another shortcoming within the respiratory system, however, that may be improved by inspiratory muscle training (IMT). Most cyclists are familiar with the benefits of doing squats and deadlifts to strengthen quadriceps and hamstrings. Respiratory muscles are also skeletal muscles that can adapt to training. The lung itself is overbuilt with respect to capacity and does not adapt to training, but the skeletal muscles used to inflate the lung are not overbuilt and can adapt to training.
A 2006 study revealed that work output by respiratory muscles during sustained heavy exercise may limit performance in elite cyclists. Dempsey et al. “unloaded” the work of breathing using mechanical ventilation, and observed cyclists had improved endurance and sustained higher power outputs, but did not improve VO2max. This study suggests that respiratory fatigue of the diaphragm or supporting inspiratory muscles may impair ventilation by reducing effective gas exchange (2), or by “stealing” blood flow from working leg muscles (4).
IMT may play a small but important role in improving gas exchange by improving the fatiguability of respiratory muscles. In a 2002 study, highly trained cyclists performed 6 weeks of IMT (30 breaths, 2 x day) and showed ~5% improvements in simulated time trial performance and reported decreased perceived breathing effort. A 2012 meta-analysis reports IMT consistently improved performance in recreationally trained athletes, ~2–5% in time trial performance, increased time to exhaustion, and reduced breathing effort. However, the effect is smaller and less consistent in highly trained athletes. A 2018 systematic review concluded benefits of IMT are most notable when ventilatory loads are high (altitude, heat, sustained near VO2max efforts).
IMT is not a large investment in time or equipment, and it certainly won’t hurt. Dr. Dempsey summarizes this well in this quote from Is the Healthy Respiratory System (Always) Built for Exercise?
“Accordingly, under special circumstances, functions of the lung (in the highly trained) and/or the respiratory muscles (in trained and untrained) will impede performance. However, the major, universal contributors to exercise performance limitation in health reside primarily in the relatively ‘weak links’ to O2 transport and utilization provided by limitations to skeletal muscle blood flow and O2 utilization by skeletal muscle.”
Bottom line: keep pushing the pedals. The cardiovascular training adaptations are where the big gains lie.
Measures and Metrics: Take Another Breath
Breathing Frequency: Mania or Madness?
I hope you have caught your breath after reading the riveting review of respiratory anatomy and physiology. It was a necessary precursor to a meaningful discussion on the application of breathing frequency as a metric for exercise intensity.
Thus far in our exploration of measures and metrics, we have reviewed RPE and HR as markers of internal stress in response to load. What does breathing frequency add to monitor load except for another metric to keep track of? Hold your breath…. it is exciting.
There is some subjectivity that can’t be escaped using RPE, and it does rely on effectiveness of self-assessment which is particularly challenging for beginners, or cyclists in the thick of competition. There is good data to confirm that breathing frequency is tightly coupled to RPE. In addition to being a more objective measure, breathing frequency can change more rapidly in response to stochastic efforts, like big climbs or sprints during an otherwise steady effort. A rider may have difficulty describing RPE as the difference between 9 and 10 cresting a hill, while breathing frequency responds instantaneously and can be measured in smaller units than the Borg scale.
Does breathing frequency offer any more insight into response to load than heart rate? Maybe not more insight, but clearer insight. Breathing frequency is not confounded by sleep, hydration, and heat, making it a “purer” measure of stress in response to the watts being generated.
From a practicality standpoint, breathing can be used to help athletes monitor exercise targets or zones more readily as it does not have a lag like heart rate response. Ventilatory thresholds (VT) are described by changes in minute ventilation (tidal volume x breathing frequency) during exercise intensity (see graph). If an athlete can carry on a conversation while cycling, they are below the VT1 turn point (talk test). These workouts would be valuable for active recovery and endurance type work (Zones 1 and 2). An athlete who is unable to speak in continuous sentences, stringing together single words strung together by forceful exhalations, would be at or near VT2. Just below this, an athlete would be working in sweet spot or at threshold. Above that, whereby words were replaced by gasps, the athlete is likely doing VO2 efforts in Zone 5.
Ventilatory thresholds VT1 and VT2 have practical application for athletes to identify work rates. Zones are depicted by shaded yellow columns.
Wait… these thresholds look familiar. VT1 and VT2 have a very special relationship with lactate thresholds (LT). The graph above and below should look very similar with exercise intensity on the X axis. The dependent variable on the Y axis has changed from minute ventilation to blood lactate.
Lactate thresholds LT1 and LT2 require blood analysis.
The third graph includes both variables as they increase with work rate. Note the two “turn points”, ventilatory threshold 1 (VT1) and VT2 and lactate threshold 1 (LT1) and LT2, occur nearly at the same exercise intensity. Measuring blood lactate is tricky, uncomfortable, invasive and certainly inconvenient if not done in a lab. The metabolic events that increase blood lactate also increase hydrogen ions (H+), which is a driver for ventilation, making breathing frequency an easier metric to record (if you have a sensor) or be aware of.
VT1= ventilatory threshold, VT2= respiratory compensation, LT1= lactate threshold, LT2= onset blood lactate accumulation (OBLA)
Perhaps the most exciting potential for breathing frequency is prediction of failure, allowing an athlete to ride close to the sun without getting burned. This is something HR cannot predict.
Most athletes are familiar the idea of calculating heart rate reserve (HRR) to describe zones of training. HRR is found by subtracting resting HR from HRmax, and then using a percentage of HRR to provide training targets. HRmax is not affected by training, and decreases with age. Resting HR decreases in response to training. Therefore, HRR accounts for individual differences in RHR. For example, if JoeCyclist has a HRmax of 190bpm and RHR of 70bpm, RHR= 120bpm. After training adaptations, his RHR is 60bpm, RHR= 130bpm. If JoeCylist continues to train at a target of 70% HRmax (133bpm), he will be working relatively less hard.
Breathing frequency reserve can be calculated in the same way. It is the difference between maximal breathing frequency and resting breathing frequency. The breathing reserve is larger compared to the HRR. During exercise, a lower percentage of breathing frequency is utilized. As the ratio of breathing reserve approximates HRR, reaching physiological limits is imminent. This is a powerful monitor of fatigue and tool for predicting failure to hold pace (Listen to the Fast Talk Labs podcast episode #363 with Dr. Stephen Seiler).
Cool. Can this be measured outside of the lab? Yes, breathing frequency reserve can be measured with a sensor and compared to % HRR to predict failure. Tymeware is one of several companies to keep your eye on. Visma-Lease A Bike used Tymeware technology during the Tour de France.
For non-Tour de France athletes, one more sensor equals one more investment in hardware, and one more set of metrics to keep track of. You will have to decide is a sensor is worth the investment. Don’t fall prey to marketing. Do your research. There will likely be wearables in addition to chest straps with differing comfort and reliability. Breathing frequency is fairly straightforward, but there will likely be claims to also measure tidal volume in order to get minute ventilation. Integrating these metrics into a platform, understanding norms and ranges and response patterns will all take a toll. Measures and metrics: mania or madness? Keep it simple. Just breathe.
What if we just simplify things and be aware of our breathing? Simple, and for most athletes, sufficient. As an exercise physiologist and coach, I cannot over emphasize the power of this very simple tool. It is bullet proof. Unlike HR, it is not subject to the influences of sleep, hydration and heat. Nor does it have a delay, such that when you are trying to achieve a max sprint for 20 seconds on: 10 seconds off, breathlessness is nearly instantaneous while HRmax is never achieved due to the lag and recovery time. It is driven by the centers in the brain very similar to RPE, but removes the subjective component.
Having athletes be aware of changes in ventilation to stay within their desired zone and monitor recovery from an interval is a powerful tool. And free. Nobody can “fake” breathing. If you are gassed, you need to suck air. And if you aren’t gassed and feign fatigue in hopes to lure another rider into doing the work, you’ll likely hyperventilate, blow off too much CO2 and quickly restore normal ventilation. The BS meter on breathing is tightly regulated.
Breathe responsibly.
Measures and Metrics: Take a Breath
In our Metrics and Measurements: Mania or Madness series, let’s take a breath. For decades, yogis and meditation gurus have focused on breath for mindfulness and relaxation. Is there merit to focusing on breath as a way to monitor exercise? Yup. There sure is, and while it may be trending in wearable devices, it isn’t new to exercise physiologists. Breathing as a measure of exercise intensity relates to cardiovascular and metabolic load. Breathing rate, as it turns out, is a key factor in your RPE.
Before diving into breathing as a tool to monitor exercise intensity (topic of the next newsletter), it might be helpful to learn or review some respiratory anatomy and physiology. As we saw with RPE, there is more behind understanding the measure or metric than a number.
A BREATH BY ANY OTHER NAME
The physical process of breathing, moving air into the body through inhalation and out through exhalation, is called ventilation. The actual exchange of gas at the cellular level is called respiration. The terms inspiration and expiration can be used to represent both ventilation and respiration (in and out of the body, in and out of the cell, respectively).
Ventilation or breathing frequency (breaths per minute) is a measurement if taken directly at the mouth, or a metric if derived from a wearable sensor. Determining respiration at the cellular level requires a metabolic cart and is a metric, calculated from measuring gas concentrations at the mouth as a proxy for the cell.
Structures of the Respiratory System
The respiratory system structures include the lungs, airways (upper and lower respiratory tracts) and diaphragm muscle. You’ve likely experienced an upper respiratory tract infection. This refers to the large airways of the nose (nasal cavity), mouth (oral cavity), sinuses, throat (pharynx) and voice box (larynx). The lower respiratory system is made up of the wind pipe (trachea), 2 primary bronchi, and the respiratory tree (secondary and tertiary bronchioles) terminating in the air sacs (alveoli). The phrase “it went down the wrong pipe” refers to food or drink making a wrong turn into the trachea rather than heading south to the stomach through the esophagus.
Fascinating facts about the structures:
The lung is the only organ to receive 100% of cardiac output and therefore is serviced by a very low resistance vascular system
Throughout the entire respiratory tree, O2 and CO2 gas exchange only occurs between the blood-gas interface in the alveoli
Transit time for gas exchange between the alveoli and capillary blood is less than 1 second. Even shorter with exercise (0.6 sec). Luckily, the structure is designed for function.
The blood-gas interface is very thin (~ 0.2-0.3 mm)
There are roughly 500-700 million alveoli and their surface area occupies half a tennis court (70-100 m2)
Capillaries that surround the alveoli can increase their capacity threefold during exercise, which protects the transit time for gas exchange
The diaphragm is a dome shaped muscle that contracts to create a negative pressure in the thorax, creating a vacuum to suck air in. Ancillary inspiratory muscles, such as the intercostals, assist the diaphragm.
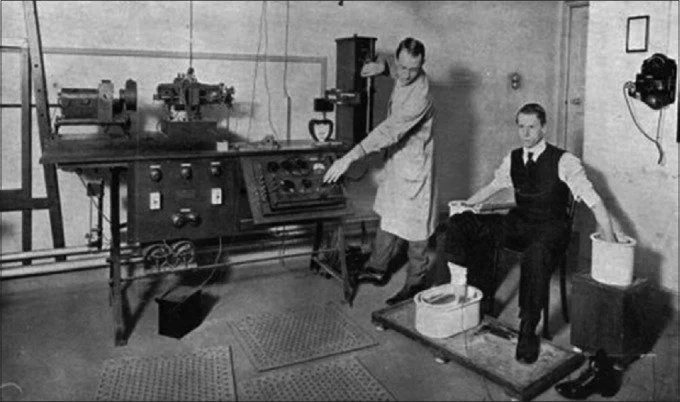
Negative pressure was the principle behind the Iron Lung, developed to treat respiratory muscle paralysis during the poliomyelitis epidemic in the 1920s and occasionally used in patients suffering from tuberculosis.
Ventilators and CPAP machines used to treat sleep apnea use positive pressure rather than negative pressure (forcing air in versus sucking air in), which are more convenient than the Iron Lung but do not mimic natural breathing mechanics.
Exhalation is largely a passive process, relying on the elastic nature of the alveoli and springiness of the rib cage to expel air. This is brilliant, allowing less energy required for exhalation.
The lung doesn’t adapt to training! Athletes may say, “my legs were fine, but I need to get my lungs into shape”. Is that accurate? There is plenty of oxygen in the lungs waiting to be picked up. That feeling of breathlessness is due to lack of oxygen being delivered to their working muscles. Training adaptations to the cardiovascular system allow oxygen to be picked up and delivered to working skeletal muscles, which also adapt to better utilize oxygen.
Functions of the Respiratory System
The primary function of the respiratory system is gas exchange, bringing oxygen in to the body and removing carbon dioxide. During the process of ventilation, several important secondary functions occur: 1) filtration and humidification of air and 2) sense of smell upon inhalation, 3) voice production through exhalation, 4) maintenance of acid-base balance, and to a smaller extent, 5) thermoregulation.
Fascinating facts about the functions:
The nose and rest of the respiratory hose is your first line of defense against bad stuff. Cilia (small hairs) and mucous work together to trap and move debris. The body produces up to 1L of mucous per day to get the job done. Go goobers!
The nose filters out particles larger than 0.5 µm, trapping it in mucous, which is then moved to the throat and into the gut by the cilia. During Covid, masks were implemented as they can filter out much smaller particles (N95 0.3 µm).
Heat and humidity. We might not appreciate the need for heat and humidity in July, but winter is coming. From the nose to the throat, air is warmed (average room temp 20°C) to 35°C (95°F) and humidified. By the time it reaches the delicate alveoli, is has reached body temperature 37°C and 100% relative humidity, preventing damage and inflammation to those delicate tissues.
Breathing requires little energy cost, ~5% of resting oxygen consumption at rest.
The lungs work in concert with the kidneys to maintain acid-base balance of pH 7.4. A rise or drop of 0.1 can have devastating effects on function.
Many animals pant to maintain body temperature. Humans can’t pant, so fortunately we have sweat glands for more robust thermoregulation.
Stimulus to Breath
There is more to breathing than you might think. If you have a healthy respiratory system, you likely DON’T think about breathing. If you have asthma (or many other diseases of the respiratory tree) you most likely think about your next breath. It is both an autonomic and conscience function.
Similar to our beating heart or digestive tract, breathing is largely an automatic function. There are inspiratory and expiratory centers located in the brain which receive chemical and mechanical sensory information, and use that to drive the diaphragm and other ancillary inspiratory muscles.
Chemoreceptors detect and ensure chemical balance (pH) and homeostasis. Surprisingly, perhaps, low oxygen is not the primary driver to take a breath. Recall that carbon dioxide is an acid: too much CO2 is our major driver to breath.
Have you ever tried to hold your breath (hypoventilate)? What happens? You take a breath before anything really bad happens! CO2 builds up, chemoreceptors tell the brain to breath and you do, despite your best effort to hold out for a few more seconds. You can’t override the body’s built in safe guard to keep you breathing.
You CAN override the system to breath more than necessary (hyperventilate). You may have experienced this during a period of high anxiety, before the start of a race or other stressful episode. Again, your body has a safeguard against expelling too much carbon dioxide just as it does retaining it. Low CO2 levels causes your blood vessels to constrict, decreasing blood flow to the brain until, leading to dizziness and ultimately fainting. One way or another, your body will succeed in slowing down breathing to restore acid-base homeostasis! Pretty cool.
There are also mechanoreceptors in skeletal muscles that drive the inspiratory center, and stretch receptors in the lungs that drive the expiratory center. Makes sense, right? Each pedal stroke triggers a mechanical sensor that feeds that information forward to your inspiratory center. Hey, my quads are working hard, send oxygen! Your lungs fill, and trigger a breath out (remember, the lung gets stiffer as it gets fuller, so is makes sense energetically not to fully inflate). Brilliant.
Breathing Response to Exercise
Minute ventilation (VE) is the amount of air breathed in liters per minute. Minute ventilation is the product of tidal volume (volume per breath) and breathing rate (breaths per minute). This is very similar to cardiac output, which is the product of stroke volume and frequency.
Average values for a 70 kg human
As the demand for CO2 removal and O2 increase with exercise, minute ventilation increases by increasing both tidal volume and frequency. The body is very smart about how to titrate the increase in these two variables. Note in the graph below how volume increases first, followed by rate. Like most everything in the body, there is a reason for this sequence.
Tidal volume: volume of air per breath. Tidal volume at rest is approximately 500 ml (based on a 70kg human). With exercise, this may increase up to 3 L/breath. Increasing minute ventilation by increasing tidal volume is a smart business move. There is a “tax” to pay with each breath called dead space. Regardless of the volume of the breath, there is an amount that cannot be exchanged. This is similar to a fee to make a withdraw from an ATM machine. If you take out $10 or $100, you pay a fee of $2 which is “lost”. Most people take out a larger sum to make the fee relatively smaller.
The lung is seemingly overbuilt, as max exercise yields ~80% of total lung capacity. You might wonder, why not take the biggest breath possible?
Mechanically, the stiffness of the lung becomes greater at higher volumes, making the metabolic cost of the work of breathing higher. There is also the ventilatory to perfusion ratio (V:Q) to consider. This basically says that each part of the lung is not equally perfused by blood vessels. The same volume of air in one portion of the lung may not be perfused as well as another, such that more air to that region will yield less gas exchange. Complicated, right?
Breathing frequency: breathes per minute. During exercise, frequency can more than double from ~12-20 breaths/minute to 60 bpm. Why not keep pushing the frequency? The metabolic cost of breathing can become significant. Similar to pedaling cadence, a faster breathing rate becomes metabolically inefficient. In revolutionary work by University of Wisconsin’s world-renowned exercise physiologist, Jerome Dempsey, the concept that the lung is not a limiting factor in exercise was challenged (Classical Perspectives). While undeniably true that its capacity is not reached during maximal exercise, the work of breathing at some point becomes significant enough to “steal” blood from working muscles (those pushing the pedals).
Digest those bits of respiratory anatomy and physiology. Understanding a basic breath is no simple task. Next month, we will explore using breathing as a tool to monitor exercise intensity and discuss some of the research around training breath to enhance performance.
Measures and Metrics: Rated Perceived Exertion
June 2025
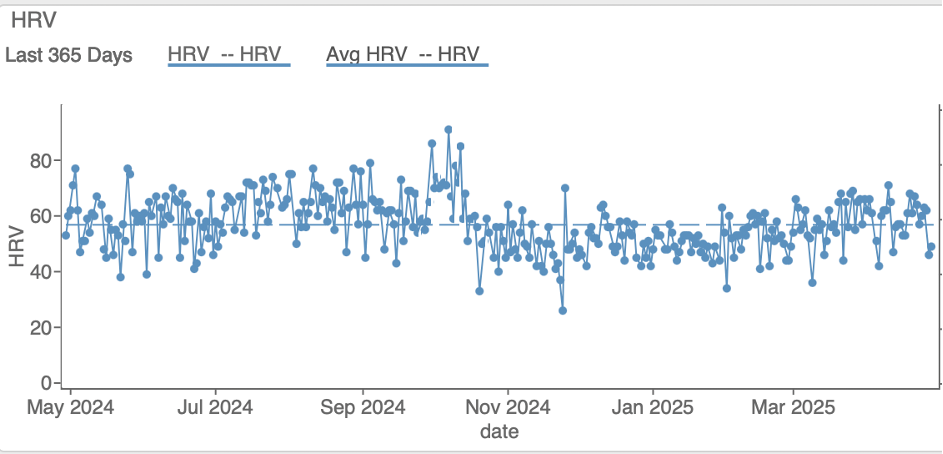
Welcome back to our discussion of measures and metrics. Last month, we discussed heart rate (HR) and heart rate variability (HRV) and how to use them to guide training. Where we should have started, perhaps, is at the beginning with rated perceived exertion (RPE).
RPE may not seem as earth shattering for training guidance as the first battery-operated monitor in 1977 (invented by Seppo Säynäjäkangas, who later went on to found Polar Electro, and released the first wireless HR monitor in 1982). Indeed, the convenience of recording HR with a chest strap was a major game changer for athletes. Imagine pedaling attached to a string galvanometer. But I would argue that creating a valid and reliable RPE scale was also ground breaking work.
Prior to chest straps, watches or rings, RPE was one of our favorite things. The RPE scale was developed in 1960 by the Swedish researcher, Gunnar Borg (who recently passed away in 2020 at the age of 92). RPE is rooted in the field of psychophysics, which is predicated on deciphering the complicated relationship between physical stimuli (like exercise) and subjective perceptions of that stimuli on sensory receptors.
Badger Connection: in 1967, Borg started visiting the US to collaborate with Exercise Physiologists, amongst them, Dr. William P. Morgan at University of Wisconsin-Madison. When I entered my doctoral program in the Department of Kinesiology in 1997, Dr. Morgan was a faculty member. It wasn’t until doing a bit of digging for this newsletter that I discovered his involvement with the Borg scale. And it wasn’t until writing this newsletter that I had any real appreciation for the Borg scale as ground breaking work.
Borg pioneered the application of the Harvard experimental psychologist Stanley Smith Stevens’ power law to the study of cycling. In his 1982 paper, Psychophysical Basis of Rated Perceived Exertion, he boils down cycling’s pain cave to the formula R= a + c(S-bn).
With the liberties, I translated it to mean R= hurt rating, S= watts. The constants (a,b,c) are things I can’t explain.
Borg used that exponent, n=1.6, to formulate how RPE increased with power, but also with sensations like “aches and pains” from working muscles, heat, anxiety and age (1985 publication). It is more sophisticated than that, but you get the gist.
I learned that Borg had at least two prior descriptor scales, 7 and 21-point, before the classic 6-20 RPE scale emerged. Observations were made in young (~20-year-old) subjects that exercise intensity of RPE 17 corresponded to a HR of 170 bpm. Max HR was ~200 bpm, and 10% of that peaked the scale at 20. Resting HR was ~60 bpm, so 10% of that started the scale at 6. Bingo! It was simple math to adjust the descriptors of the 21-point scale to the new 15-point (6-20) scale.
This linear category scale allowed comparisons with HR, respiration rate, blood lactate, and oxygen consumption (VO2) which have proven valid (see 2002 meta-analysis).
These images, taken from a 2013 study, illustrate the relationship between RPE, blood lactate and VO2.
This study concluded, “Borg's RPE seems to be an affordable, practical and valid tool for monitoring and prescribing exercise intensity, independent of gender, age, exercise modality, physical activity level and coronary artery disease status.” Brilliant! Affordable, practical, accessible to anyone and everyone, and doesn’t require an app, updates or even electricity.
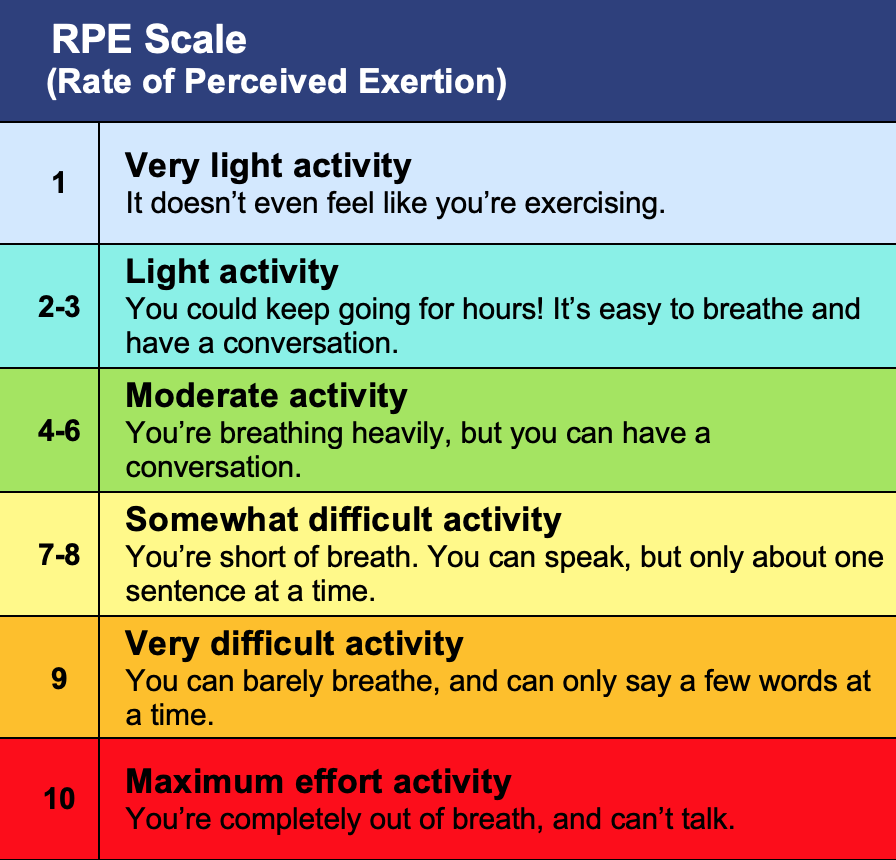
There was an update in the form of a category ratio (CR) modified Borg scale from 0-10. This scale is used more frequently to rate response to a treatment, or to describe a sensation, such as shortness of breath (dyspnea) during an activity. This is a good segue into ventilation as a measure of exercise intensity, a topic for a future newsletter.
CR Modified Borg Scale
It is no surprise that the American College of Sports Medicine (ACSM) recommended RPE in their Guidelines for Exercise Testing and Prescription in 1986, where is has remained steadfast for the past four decades. Or that they wrote a legacy piece from which I borrowed heavily.
There are skeptics who resist using a subjective rating to describe a physiological state. And to this, Borg responded, “Neither a single RPE value nor a heart rate measure may be used alone as an accurate indicator of ‘dangerous strain.’ They complement each other. Studying fatigue and exertion only from a physiological perspective is as impossible as dealing with color, emotion or motivation in primarily physical or only physiological terms. That is, exertion and fatigue are states with both physiological and psychological aspects.”
As a coach, I find the Modified Borg scale really helpful in communicating with athletes.
Using the Zone Model to describe training intensity, the modified Borg can be used instead of or in conjunction with HR and power.
Like cardiac drift, there is RPE drift with prolonged exercise at a given power output. This is important when communicating a “zone” with an athlete. For example, if the athlete is instructed to hold threshold power of 200W for one hour, the load (watts) remains the same. If the athlete cannot measure power output, they may choose to measure HR or RPE. In this case, threshold corresponds to RPE 5-6 and a HR of 90% max. Over time, there may be cardiac drift, such that HR increases to a higher % of max. And RPE may creep upwards as that athlete experiences muscle discomfort, increase in temperature, blood lactate, increased ventilation, and other factors. If the athlete backs off to maintain a HR of 90% max and RPE of 5-6, the training stimulus (power) is not achieved. It is important to recognize, when describing training intensities, that HR and RPE are responses to load. They can be used to describe an initial load, but they will drift higher than the initial load over time. Similarly, HR and PRE at baseline can be affected by a multitude of factors: hydration, sleep, stress to name a few. If an athlete wakes up with an elevated HR and RPE 2-3 before brushing their teeth, it might be time to consider lowering the training load. This is where coaching and training is both a science and an art, and Borg was both an Einstein and a Picasso. My appreciation for this scale has reached a 10.
Measures and Metrics: Mania or Madness? Heart Rate and Heart Rate Variability
May 2025
Do you remember the days, or maybe are still enjoying them, when you simply went out for a bike ride? If you have gotten caught up in measures and metrics, your pre-ride routine may be a bit more complicated than merely checking your tire pressure (and tire pressure has evolved from riding 120 psi on 23mm) and Cat Eye computer. For those too young to remember, those revolutionary bike computers were hard wired with a cable running from your fork up to your computer mount on the handle bar, secured with zip ties, hopefully connecting without physically touching the sensor precariously attached to a spoke, calculated your average speed and total distance. In modern times, you are likely securing your HR monitor chest strap, ensuring good connectively by spitting on the electrode, firing up your Garmin/Wahoo and trying to recall the steps (for the hundredth time) to upload a course or workout, and calibrating your power pedals (after remembering that you forgot to put in new batteries). And that’s after reviewing all of your sleep, heart rate variability, stress level and body battery metrics to determine your training readiness. I rather miss those days when I just checked in with how I felt. After the criterium cornering clinic on Sunday (thanks to Reece Linder at Ascend Performance), my Garmin noted that I needed 60 hours of recovery. Really?
The questions top of mind are these:
What is the difference between a measure and a metric?
What do these measures and metrics mean? The May newsletter is the first in a series of measures and metrics, with a focus on heart rate and heart rate variability.
How do I use measures and metrics to guide my training?
Measurements versus Metrics
Measurements are made, metrics are created, derived or estimated from measurements. Measurements need to be valid and reliable. Validity means the measurement actually measures what it claims to measure, and does so accurately. Reliability is consistency of that measurement in similar conditions. If the measures aren’t valid or reliable, the associated metrics are even less so. Let’s dive into heart rate (HR) and heart rate variability (HRV) to illustrate the difference between measures and metrics.
Heart Rate
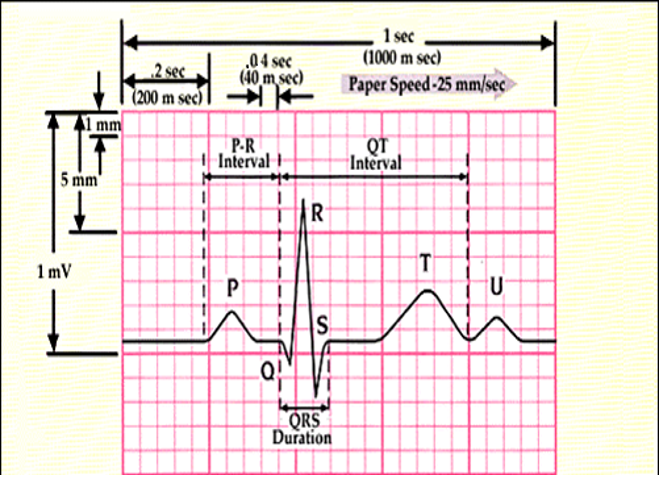
HR is the number of times your heart pumps blood per unit of time, expressed as beats per minute (bpm). You can measure HR by putting a finger to your carotid, brachial or radial artery and counting beats for 60 seconds. Your physician might order a test called an electrocardiogram (EKG) to measure the electrical activity of your heart. An EKG maps out the time intervals between electrical events of the atria and ventricles (chambers of the heart) to diagnose arrhythmias or ischemia. Below is a sample strip of what the electrical activity looks like in a normal cardiac rhythm, along with labels of the specific waves and intervals.
Normal EKG
Waves and intervals
Somewhere in between these methods, athletes can determine HR by wearing chest straps, wrist straps and rings. Chest straps use an electrode sensor to measure the electrical activity of the heart, similar to an EKG. Wrist straps and rings use an optical sensor to measure changes in blood volume under the skin (hence the light that shines under your watch or ring) called photoplethysmography (PPG). HR can be deduced by the time between changes in blood volume. I would argue that this is a metric more so than a measure.
Garmin HR strap and Instinct watch
Optical technology is subject to error due to motion artifact (the sensor moving on the skin) and signal crossover (repetitive motions in running or cycling are misinterpreted as the periodic signal of interest). According to one study, error increased up to 30% with activity (Apple, Garmin and Fitbit devices, not all are not all created equal) compared to rest. Specifically, the sensors tested were 4-10 bpm off compared to EKG testing at rest, and up to 20bpm off while walking (not even vigorous activity).
Key Point: chest straps measure HR through electrical signal and are more accurate than wrist straps, which deduce HR and are prone to error through artifact and signal crossover. Heart rate readings at rest are more reliable than during exercise for PPG devices.
What do resting and maximal HR numbers mean?
The heart is our most amazing muscle. It can beat on its own, without input from our brain. In the case of a heart transplant, only the vessels are reconnected to the donor heart, not the nerves, and yet the heart beats and effectively changes pace in response to hormones. Although it can beat to its own drum, the heart is innervated and controlled by the autonomic nervous system (ANS). There are two branches of the ANS: sympathetic and parasympathetic. Sympathetic is often referred to as “flight or fight” and parasympathetic as “rest and digest”.
Heart rate tells us how much influence comes from those branches of the ANS. Left without innervation, it would beat on its own around 100bpm. The lower that number, the more the parasympathetic system is pumping the brakes. The higher the number, the more the sympathetic system is hitting the gas in response to some flight or fight stimulus, like exercise.
Monitoring heart rate has implications for cardiovascular health and monitoring exercise. Resting heart rate (RHR) in adults has a wide range from 60-100bpm. A HR below 60rpm is called bradycardia and above 100bpm is called tachycardia. Simply stated, slow and fast rates. A low RHR is an indication of cardiovascular fitness. Some endurance athletes have non-pathologic bradycardia in the low 40s.
HR can be affected by posture, sleep, stress, pain, caffeine, nicotine, and heat. Therefore, it is best practice when tracking RHR to do so upon waking. A drop in RHR may be a positive sign of adaptions to training. An elevated RHR may indicate onset of illness or dehydration.
While RHR provides insights into cardiovascular health, maximal heart rate (HRmax) is much less interesting. HRmax invariably goes down with age, starting roughly around age 25 at a rate of ~1 beat per year. HRmax is not a reflection of fitness, although determining HRmax is important for setting training levels or zones. It can be estimated with formulas but it is more accurate to find your HRmax with a field test (unless you have the means to test in a lab with a metabolic cart).
· [220-age] is the most common and inaccurate)
· [207- (0.7 x age)] more precise for people over 40 y/o
· [211-(0.64 x age)] slightly adjusted for active people
· Warm up 5min, hard effort for 10min with last 30s all out. Average three trials with a day of rest in between.
Key Point: RHR gives insight into fitness while maxHR is a gauge of age.
How do I use HR in training?
HR during sub-maximal exercise is about supply and demand. As you pedal your bike, the demand for energy to do physical work increases. Your body responds to that demand by supplying more blood, and therefore oxygen, to working muscles. It does this in part by increasing HR.
Monitoring the response of HR to sub-maximal exercise provides powerful insights into training stress and adaptation. At rest and sub-maximal work rates, a trained person will be better adapted and able to meet the demand and therefore will demonstrate a lower HR for a given power output. Conversely, an acute decrease in HR at a sub-maximal work rate can indicate over-reaching (the predecessor to over-training).
Can I use HR to determine intensity targets, levels or zones?
Realize that HR is a measure of strain, or response to an application of load (stress). For those cyclists who don’t have the luxury of training with power meters, it is tempting to execute workouts using HR as a guide. We will save zone or level training for a future newsletter. For now, it is important to appreciate the inherent danger in setting a target HR as a means to guide your intensity. The load is what is what it is: 100W, 200W, 500W. HR is a marker of internal stress in reaction to the intensity or load placed upon it. It is NOT the load. If you are relying on HR to hit a certain target power, you might be overshooting or undershooting the target. Furthermore, recall that HR is impacted by sleep, hydration, stress, pain, caffeine, nicotine, and heat. HR cycling at 200W at 60 degrees is going to be lower than cycling at 200W in 90 degrees.
Should I use HR as a surrogate for VO2max to monitor training?
Increasing oxygen consumption is a well-orchestrated dance with the respiratory and cardiovascular systems partnering up to increase ventilation, heart rate and intensity of pumping, and redirecting of oxygenated blood to the working muscles.
Oxygen is used in a clever combustion chamber called the mitochondria to burn fats and carbohydrates to provide energy in the form of adenosine triphosphate (ATP) to working muscles. The rate of work (think power) is matched in a linear fashion by oxygen consumption (VO2) until a maximal point (VO2max) is reached. Power can still increase, but beyond VO2max, energy is derived from non-oxygen or “anaerobic” sources.
VO2max is the gold standard for assessing cardiovascular fitness. Measuring oxygen consumption requires lab testing with a metabolic cart, which is expensive and not practical for most athletes. Due to the linear relationship of VO2 and HR with work rate, devices often use HR as a surrogate for estimating VO2 max.
After conducting hundreds of VO2max tests in the lab, I can assure you it is an estimate calculated by proprietary algorithms and not a true measure, although perhaps an interesting metric. The chart below, generated in Garmin Connect, is a good example of how HR data is used to estimate VO2max.
Key Points: a decrease in sub-maximal HR response to a given work rate is a key indicator of chronic fitness adaptation or acute over-reaching. Caution should be exercised when using HR to target load, as it is an internal measure of stress to a load. Training HR can be used to estimate VO2max. That metric does not predict performance.
VO2max is the gold standard for assessing cardiovascular fitness. Measuring oxygen consumption requires lab testing with a metabolic cart, which is expensive and not practical for most athletes. Due to the linear relationship of VO2 and HR with work rate, devices often use HR as a surrogate for estimating VO2 max.
After conducting hundreds of VO2max tests in the lab, I can assure you it is an estimate calculated by proprietary algorithms and not a true measure, although perhaps an interesting metric. The chart below, generated in Garmin Connect, is a good example of how HR data is used to estimate VO2max.
Key Points: a decrease in sub-maximal HR response to a given work rate is a key indicator of chronic fitness adaptation or acute over-reaching. Caution should be exercised when using HR to target load, as it is an internal measure of stress to a load. Training HR can be used to estimate VO2max. That metric does not predict performance.
Heart Rate Variability
HRV is the variation in time between beats, measured by the R-R interval on an EKG reported in milliseconds (ms). It is a metric. The actual interval is measured between beats is measured, but the variability number is calculated using an algorithm.
Recall that a chest strap utilizes a sensor to read electrical activity, whereas wrist straps and rings use optical sensors and PPG, which are prone to artifact. Technically, these devices measure pulse rate, not HR, if you want to get snippy about it. Which apparently, I do, because that measure is now put into a calculation to come with a metric, HRV, so it should be valid and reliable.
To further muddy the waters, HRV calculations are often (always?) proprietary. This is above my pay grade as it involves math, my nemesis. The calculations can be time-domain or frequency-domain methods, as described in the table below.
Key Point: HRV is a metric calculated from a measuring an electrical signal from the heart. How that signal is measured (electrode or PPG) will impact the accuracy of the number. The actual number is a metric that comes from a proprietary algorithm, so cannot be compared across devices.
What does HRV mean?
Remember that the heart is innervated by the parasympathetic (vagus nerve) and sympathetic (cardiac nerves) of the autonomic nervous system. The balance between these branches is called “tone” and is reflected in HRV, with a high HRV being an indicator of health.
Tone responds to many variables, including exercise and stress. Increased sympathetic tone increases HR. Perhaps a bit counterintuitive, increased sympathetic tone decreases HRV. Think about it in terms of flexibility: if the gas pedal is all the way down (sympathetic tone), there is little variation in speed (heart rate). When the foot is on the brake (parasympathetic tone), there are fluctuations in speed just be removing the brake, and even more by hitting the gas. This leaves the body more flexible to adapt to internal and external stimuli.
A 2020 study by Tegegne et al., used 10 second resting EKG measurements to establish references for HRV based on age, sex and fitness.
Key Point: The autonomic nervous system with sympathetic and parasympathetic branches impacts all systems of the body. Tone is a reflection of the cardiovascular, digestive, respiratory and other systems ability to react and adapt to stimuli. A higher HRV is an indicator of overall systemic health.
How do I use HRV in training?
Since HRV numbers are generated from non-disclosed secret sauce algorithms, comparisons between devices are meaningless. I found this graph from LifeHacker very helpful in visualizing the different ranges in HRV and RHR based on several common devices (Whoop, Oura, Apple Watch, Fitbit and Garmin).
This is important for coaches to understand, as they may be looking at HRV data from many athletes using various devices. And for athletes using one device, it is important to understand that reference norms were established using gold standard EKG measurement of the R-R interval, not PPG.
However, not all is lost. The cyclist looking at HRV from one device can gain insights into their training by ignoring absolute numbers and following trends. Here is an example of an athlete’s HRV tracked over the course of a year. She had a 100-mile gravel race in October. During the taper, HRV was at its highest, and then dramatically dropped the day following the event. Slowly, through the off season and pre-season, it has climbed back up to baseline.
Key Point: HRV is an indicator of autonomic nervous system tone and overall health. In general, a higher number reflects more “flexibility” of the system to adapt. This number should not be compared across devices. Reference norms provide some insight, but be mindful of the errors inherent to wearables, particularly devices utilizing PPG when drawing conclusions. Cyclists may gather information about their readiness to train by following trends in HRV using the same device with data collected at the same time of day (preferably overnight or upon waking).
Hierarchy of Movement: Strength
April 2025
Possibly the most exciting hockey game since the Miracle on Ice in 1980 was played last Sunday, with the Wisconsin Badger Women’s Hockey Team securing their place in history by earning their 8th National Championship. It was an amazing demonstration of strength, both physical and mental. Congratulations to our very own Drafter, Coach Crum, and all the players and staff on their strong win against Ohio State.
Our next chapter in movement literacy focuses on strength. We recognize that the movement hierarchy of mobility, flexibility, stability and strength are not linear steps, but rather interdependent. Prerequisite strength is the foundation upon which mobility and stability develop. From there, strength can be further developed to reach the pinnacle of the movement pyramid, performance.
The Strengths and Weaknesses of Cycling
In general, cycling is one of the “best” exercises for building cardiovascular or aerobic fitness. It is a forgiving sport for many orthopedic maladies and bionic parts (total knees and hips) due to the non-impact nature of pedaling. It is one of only a few sports that can be enjoyed by adolescents to centenarians together on the same road or trail. During the summer months, my mom and I enjoy weekly rides on the Badger State Trail. It is usually the highlight of my training.
I recently competed in a the Iola Snow Bully Fat Bike Race and was taken aback to be in the 55-99 age category. The announcer, in jest, announced the winner of the “55 to death” age group. He wasn’t wrong, but I had not stopped to think of it like that. The questions becomes: is cycling enough to promote a healthy lifespan?
Cycling has some serious limitations for overall health. Namely, the lack of impact loading which is necessary for bone health, and minimal eccentric loading, which is crucial for strength of muscle and tendon. Cycling takes place exclusively in the sagittal plane, leaving muscles and tissues in the frontal and transverse planes largely ignored, to become shortened or weakened. Strength training is therefore paramount not only for cycling performance, but for the health span of cyclists.
Surely cycling a good exercise to build quadriceps strength, right? Look at the legs of Tour de France riders Geraint Thomas, Julian Alaphilippe and Peter Sagan celebrate in this podium photo from 2018. There is no doubt cycling has built strong legs. Form follows function: the cross-sectional area of that muscle will vary dramatically based on how it is best utilized- for sprinting (Sagan in green), climbing (Alaphilippe in polka dot) or endurance (Thomas in yellow). You may or may not be surprised to learn that strength training is a big part of these quads. Peter Attia,MD, interviewed 3-time Tour de France GC champion, Tadej Pogacar, to learn how he strength trains during and in the off-season (listen here).
Unless we continually find a bigger gear to pedal up a steeper hill, there is a limit to the strength that can be gained on the bike. Strength is the amount of force (mass x acceleration) that can be produced and transferred to push or pull an object. Strength can be achieved through hardware and software upgrades.
Increased Strength: Hardware and Software Upgrades
Hopefully you are now convinced, or at least open to the idea of strength training to improve your cycling performance and extend your health span. Strength gains can happen through hardware and software upgrades.
Let’s start by talking about hardware. The architecture of muscle was reviewed in an earlier newsletter. Recall that a single muscle cell is called a myofiber (myo; Greek origin for muscle). There are ~20-80 myofibers surrounded by connective tissue to form a fascicle, and many fascicles together surrounded by connective tissue to form a muscle.
Myofibers are made up of proteins called myofilaments. The two major myofilaments responsible for contraction are actin and myosin. Myosin looks and acts a bit like an oar of a row boat, the myosin head catching actin and pulling the lever to create motion. The physical connection between actin-myosin complex is called a cross-bridge.
Strength training can upgrade the hardware by increasing the cross-sectional area through mass and volume of the muscle (hypertrophy). The number of myofilament proteins within the muscle fibers increases due to protein synthesis. Back to the oar analogy, the more oars in the water, the stronger the stroke. This is an oversimplification, but works for our purposes. Should you want to dabble further in the science of force production, this is an excellent paper that comes from Kerry McDonald (post-doctoral fellowship with my mentor, Dr. Richard Moss).
Hypertrophy occurs in all fibers (slow and fast twitch), however, fast twitch fibers have a greater potential for growth. This is a bonus for cycling AND healthy aging. Fast twitch fibers are capable of generating higher forces compared to their slow twitch counterparts. Age related loss of muscle (sarcopenia) takes a greater toll on fast twitch fibers. This is arguably the most important reason for all athletes, particularly menopausal women, to lift heavy. Fast twitch fibers aren’t only critical to win a sprint. As we age, their strength allows independent transfers from floor to chair, or picking up a grandchild.
Strength gains are also made through upgrades in software, represented by our central nervous system. These are the gains seen initially in the first several weeks of weight training, preceding and in the absence of hypertrophy. Some theorize that hypertrophy is for show and software is for go.
In order to understand the software upgrades, let’s quickly touch upon the two ways in which force can be graded. You can select a power output of 100W or 500W. That is what is meant by “graded”. This is accomplished through recruitment and summation of twitches. Huh?
1. Recruit more fibers. Muscle fibers work on the all-or-none principle. When a signal from a nerve reaches a group of muscle fibers, called a motor unit, all of the fibers in that motor unit contract fully. A motor unit may innervate as few as 10 fibers in eye muscles for fine movements or thousands of fibers in the quadriceps for pedaling. Based on your need for 100 to 1000W (okay, I’ve never hit 1000W), recruitment is based on Henneman’s size principle, which states that motor units are recruited from smallest to largest. It just so happens that the smallest motor units tend to innervate slow twitch fibers, and larger motor units innervate fast twitch fibers.
Strength training increases force production through more synchronous recruitment of fibers. Henneman’s size principle is still intact. However, rather than recruiting all the slow twitch (Type I) fibers and then tapping into the fast twitch fibers (Type II), there is less division and more synchronization of fiber type recruitment. As fast twitch fibers generate more force, this is a software upgrade that taps into hardware.
2. Summation of twitches. A nerve impulse will signal all the fibers in that motor unit to contract. But, the tension of those fibers depends on the number of cross-bridges formed. That, in part, depends on how much calcium is hanging around. The higher the frequency, the more calcium available to activate additional muscle units (sarcomeres).
Training Increases the frequency of twitches, which increases the amount calcium, which increases force. Lost? Think of the effect of a certain beverage on your system (coffee or whiskey, perhaps). If you have an impulse to take a sip every hour, that effect is VERY different than if you have an impulse to take a sip every minute for an hour. The frequency of impulses that introduce calcium into muscle is similar. Chronic training also increases calcium sensitivity, which impacts summation. Meaning, for the same amount of calcium, there is a stronger contraction. This speaks to the cooperative nature of calcium and cross bridge interaction, which is uber complicated but fascinating. Summation is one reason people tend to “prime” a heavy compound lift like a back squat or dead lift with an explosive box jump or ball slam.
How do I upgrade my hardware and software?
Acquiring more hardware is achieved by lifting lighter weights with greater repetitions to create a stimulus for hypertrophy (muscle cross-sectional area). Increasing strength through software upgrades (central nervous system) can be achieved through lifting heavier weights and fewer repetitions, creating greater muscle fiber recruitment. The balance between these basic types of lifting prescriptions changes based on in versus off-season, as well as athlete’s goals and rehabilitation from injury. For example, an athlete may adhere to a regiment of 2 x 15 at 60% 1RM in-season to maintain muscle mass, and switch to 4 x 4 at 90% 1RM in the off-season to build strength. Conversely, some strength and conditioning coaches support the reverse, recommending high reps in the off season, as this tends to cause more muscle damage (the stimulus for hypertrophy) and soreness. During the season when a cyclist does not want soreness interfering with riding, weight training moves towards less reps and software upgrades. In my practice as a physical therapist and coach, I often rely on certified strength and conditioning specialists to prescribe effective training programs, as they are beyond the scope of my practice.
Strength and Conditioning Coach: Worth the Investment
Here is my plug for Corey Digman of Digman Fitness. Please see my Community Collaboration page for further details on how to train with Corey. I’m there two days per week. Corey has agreed to post more on this topic in his upcoming blog, so check it out!
Foundational Lifts
In general, it is recommended that a strength training program include the 7 compound foundational movements: 1) squat, 2) lunge, 3) hinge, 4) push, 5) pull, 6) plank and 7) rotation. As cycling is predominantly a push activity, the tendency is to train push (squat, lunge) activities to build strength for performance. However, pull activities (rowing, dead lift) should be emphasized for muscular balance.
Functional Strength
In addition to traditional strength training, I highly recommend integration of functional training. I had the fortune of being mentored by Steve Myrland, a certified strength and conditioning specialist with experience at the collegiate and professional team levels. Steve is a student of Vern Gambetta, widely regarded as the founding father of functional training and founder of GAIN. Functional training refers to training of movement patterns, not isolated lifts, to increase efficiency and fluidity of muscle firing through three planes of movement (sagittal, frontal and transverse). Training usually involves body weight or minimal equipment, like bands and straps. Having attended functional training sessions with Steve for years, no two functional training sessions were the same. Steve agreed to share a short series of videos called “Happy Hips and Hamstrings.” There are many more in his library, and I’m sure he would be thrilled to share.
In summary, movement literacy is a hierarchy, built from mobility, flexibility, stability, strength and skill. In-season performance occurs at the peak of this hierarchy, but a lifelong commitment to movement requires the foundational building blocks, especially in the off-season. Think long term and train for life being an athlete with plasticity, resiliency, durability. Put as many tools in your toolbox as you know how to use. Establish a routine using these tools, rather than picking your favorite tool for each workout. If you find yourself with movement dysfunction, resist the whack-a-mole approach. Find a technician who can help solve the biomechanical puzzle. It may take more than one clinician to sort all the missing pieces. Lastly, exercise is medicine and our prescription will definitely change with age and is sex specific. What works today may not work tomorrow. Change is the only constant.
Hierarchy of Movement: Stability
It all begins with an idea.
March 2025
March Madness. As defined by a 46 degree temperature swing in 10 days. The Fat Tire Birkie will once again face a challenge in providing a snow packed course for all of those studs (referring to tires). Good luck to all of those drafting responsibly on the hills of Hayward next Saturday. While weather pattern instability doesn’t have an easy solution, there is lots to be done about our core stability.
Stability is the next chapter in our Movement Literacy. Stated simply, stability is our anchor point. From that predictable and unwavering foundation, we can maintain posture and alignment, resist displacement from perturbations and control movement.
It is easy to see what happens when the foundation is soft and unstable. In the human tower, where is the foundation, exactly?
Don’t worry about sounding professional. Sound like you. There are over 1.5 billion websites out there, but your story is what’s going to separate this one from the rest. If you read the words back and don’t hear your own voice in your head, that’s a good sign you still have more work to do.
Be clear, be confident and don’t overthink it. The beauty of your story is that it’s going to continue to evolve and your site can evolve with it. Your goal should be to make it feel right for right now. Later will take care of itself. It always does.
Our foundation is the lumbopelvic-hip complex. Rotation, side bending, flexion and extension are controlled by at least 58 muscles and supported by ligaments. In addition to passive stability, ligaments have proprioceptors and mechanoreceptors to give us awareness of pain and where we are in space.
Example of image-based musculoskeletal model of the pelvis, hip and lumbosacral complex. Muscles are represented as red lines connecting origin and insertion points.
Di Martino, A., Geraci, G., Brunello, M. et al. Hip-spine relationship: clinical evidence and biomechanical issues. Arch Orthop Trauma Surg 144, 1821–1833 (2024). https://doi.org/10.1007/s00402-024-05227-3
From this stable foundation, transfer of forces between the upper and lower extremities during movement can happen with precision and power. You’ve likely witnessed riders who are grossly unstable, and you can literally see the wasted watts as they struggle to keep generating power in the sagittal plane. That’s not so say those riders can’t whoop on you. During Big Sugar in October, a (much younger) woman shared in our glorious pace line for a few miles. She was strong, but grossly unstable. Ultimately, she left the comfort of the draft and speed to her place on the age group podium. I can’t help but wonder if she could have been on pro podium had she not lost so many watts due to an unstable foundation? I also wonder how many more high torque revolutions she can generate with her knees and hips traveling outside of the sagittal plane without stress, strain and pain?
There are wildly successful athletes with unorthodox movement patterns. Hall of Fame legend Babe Ruth, NBA’s Joakim Noah, PGA’s Jim Furyk to list a few. I wouldn’t be so bold or presumptuous to say “better form” would improve their standings. With cycling, the number or repetitions per minute has a different impact than the number of pitches, basketball shot or golf swings in the same period of time. In addition, a cyclist’s body is constrained at points of contact: handlebars, saddle and pedals. Aberrant motions might have a bigger price to pay as they are constrained within those points of contact. Finally, watts are watts, and they only matter most when generated in the direction of the drivetrain. Why waste them?
Stability training is typically low hanging fruit for the cyclist: the smallest investment for the biggest gains. Beyond performance, stability is one key to injury prevention and recovery. Landmark studies in the late 90s by Hodges et al. looked at core activation in patients with and without low back pain, and discovered that local stabilizers (transversus abdominus and multifidi) were delayed in those with low back pain. 2004 study by my mentor, Dr. Thomas Best, at University of WI-Madison, showed that athletes recovering from acute hamstring strains returned to sport sooner with fewer recurrence of injury with stabilization exercises compared to stretching and strengthening (more to that study, but those are the cliff notes). Together, these studies suggest that the ability to initiate core stabilizers is at the very least, an important precursor to pain free, precise and powerful movement.
A stable foundation begins with core work. I am embarrassed (again) to say that I missed or misunderstood this concept in physical therapy school. 6-pack abs certainly have a role in stabilization, but they are not the main players. The “core four” are the diaphragm, transversus abdominus, multifidus and pelvic floor.
To understand core stabilization, it is helpful to envision the abdomen as a cylinder, with the diaphragm making up the ceiling, pelvic floor muscles at the base, and the front and back walls reinforced by the transversus abdominus (TrA) and multifidus, respectively. These muscles can be strengthened and programed through neuromuscular control to fire to increase intra-abdominal pressure and spinal stabilization during exercise. Imagine the muscles shortening to increase pressure inside the cylinder, preventing the soda can from collapsing. For those who aren’t soda oriented, Boyle’s Law, PV1= PV2, might be more helpful. At the core (pun), when volume decreases due to the walls of the cylinder contracting, pressure will increase.
The diaphragm is our primary breathing muscle, so it gets a free pass for assisting with stabilization during aerobic exercise. Halting ventilation to increase the pressure in the cylinder during cycling is ill advised, although may be incredibly helpful during strength training. There may be performance benefits to training with certain breathing techniques. Pursed lip breathing, nasal breathing, and inspiratory resistance training may all have a place in performance. I would refer you to the works of one of the greatest respiratory physiologists (and teachers) of all time, UW’s very own Dr. Jerry Dempsey (one of first to show that despite the lung being overbuilt, respiratory muscles could be a limiter in performance in male endurance cyclists).
Back to our discussion of the “core four”, leaving the diaphragm to do its thing, the TrA, multifidi and pelvic floor muscles provide an anchor from which to maintain posture and alignment, resist displacement from perturbations and control movement. Exercises named after creatures, such as dead bugs and bird dogs, target core stabilizers.
Beyond the core stabilizers, there are other global (more superficial) muscles referred to as movers. It may be helpful to categorize muscles by their role so as to be more intentional in exercise prescription: 1) anchor, 2) maintain spinal posture and alignment and resist displacement from perturbations, and 3) control limb movement. This categorization is something that I’ve found helpful, but is certainly not universally recognized or approved. The anchor, as noted above are the core stabilizers made up of the TrA, multifidi and pelvic floor muscles. Global stabilizers function to maintain alignment and resist perturbations include internal and external obliques, rectus abdominus, quadratus lumborum and erector spinae. Planks, side planks, superman and crunches are examples of exercises that target global stabilizers.
Finally, global mobilizers connect the pelvis to extremities for movement include iliopsoas, rectus femoris, and gluteal muscles. Bridges (double leg, progressing to single leg), single leg squats and lunges are good exercises for global mobilizers. The line between stability and strength exercises should be fuzzy. After all, the goal is to strengthen the stabilizers in order for them to provide an anchor to strengthen the muscles that put power through the pedal. Strengthening will be the final chapter of movement literacy.
Hierarchy of Movement: Flexibility
It all begins with an idea.
February 2025
February is here with frigid temperatures. Let’s heat things up with a conversation about flexibility. Last month we talked about mobility and the 3 F’s: moving freely and fluidly through a functional ROM. Using a cycling analogy for joint mobility, compare the feeling of pedaling with an old worn, rusty chain to a new lubricated one. The total amount of movement may be the same, but the quality of that motion is very different.
Flexibility is one component of mobility. It is defined as ability of muscle, tendon and fascia to lengthen passively (in the absence of muscle contraction) through ROM. Flexibility is often limited in muscles and their respective tendons crossing two joints (bi-articular). The hamstring muscles, crossing both the hip and knee joints, are a great illustration of flexibility impacting mobility at the knee joint. A cyclist may have excellent knee mobility, fully straightening (0° extension) and bending until the heel contacts their butt (~130° flexion). However, when placed in a supine position with the hip flexed to 90°, knee motion stops 20° short of full extension (can’t straighten to 0°). What changed? In 90° of hip flexion (think about sitting on the saddle), the hamstring muscles, tendon and fascia are put on stretch across the hip joint. If there is limited flexibility, there isn’t enough length in those tissues to also allow the knee to fully extend. “So what?”, you might ask. So… what happens when you want to really drop into a more aerodynamic position? With adequate hamstring flexibility (length), the pelvis rolls into an anterior tilt and the spine follows to maintaining alignment. If there isn’t adequate length available, the pelvis is “tethered” and the desired aerodynamic effect is achieved through spinal flexion, placing high stress on the lumbar discs. You’ll save those previous watts, but at a price.
Is stretching the answer? The efficacy of flexibility exercises (stretching) on improving ROM, injury prevention, and their negative impact on muscular performance in explosive sports has been widely discussed in the literature. Like most recommendations, “it depends”. Stretching recommendations for the hip flexors of a cyclist may be dramatically different from those of a gymnast. Stretching may be contraindicated after an acute muscle strain, but warranted after 6 weeks of an immobilization for an ankle fracture. Stretching may minimize muscular explosiveness in a 100-meter but enhance muscle function in a 100-mile road race.
What exactly are we stretching? I’m somewhat embarrassed to admit that it took me longer than it should have to appreciate stretching targets more than just the muscle, or contractile tissue. Indeed, stretching increases the distance between the actin and myosin myofilaments (muscle proteins responsible for shortening or contraction) in each sarcomere (functional contractile unit of muscle), allowing the muscle fiber to elongate. Once the fiber reaches its maximal resting length by stretching the actin and myosin and other proteins such as titin, of each sarcomere, the target becomes the connective tissue. Each muscle fiber is surrounded by connective tissue (endomysium). Groups of fibers are arranged into fascicles, also surrounded by connective tissue (perimysium). Finally, all the fascicles of a muscle are enveloped in connective tissue (epimysium). Muscles are connected to bone via connective tissue (tendon) at the musculotenidous junction. Stretching, therefore, is much to do about connective tissue.
Muscle and connective tissue
Take your time stretching. Muscle and connective tissue are viscoelastic materials, which have rate and time dependent properties. Think about silly putty. If the goal is to stretch silly putty, the rate at which you load the silly putty will be important for its deformation behavior. The more quickly you pull or stretch the silly putty, the less deformation compared to a slower rate. The take home: a slower rate of stretching is likely more effective than a rapid, bouncing type approach. Once you have the silly putty (tissue) under tension, two magical things happen with time. If you were to hold the stretched silly putty at a constant length, the material would begin to exhibit less tension (stress relaxation). You’ve likely felt this after ~20s of placing your hamstring on stretch. Without gaining any more ROM, there is a sense of less tension. Similarly, if you were to exert a constant force on the silly putty to lengthen it, the material would eventually lengthen (creep). You might have trouble getting the silly putty back into the container. Of course, silly putty isn’t the same as muscle, tendon and fascia, but it provides a framework to understand the properties of viscoelastic material and why stretching is best accomplished at a slow rate with time (~20-30 seconds) under tension.
The literature is fairly clear that acute stretching increases stretch tolerance, stress relaxation and creep. What stretching doesn’t seem to do is decrease mechanical stiffness. And that’s good! Right? The word “stiffness” used amongst engineers and clinicians may not mean the same thing, exactly.
The Merriam-Webster dictionary defines stiffness as “lack of suppleness or flexibility.” We defined flexibility as the ability of muscle, tendon and fascia to lengthen passively (in the absence of muscle contraction) through ROM. A patient might report feeling “less stiff” after performing a hamstring stretching routine. The clinician measures increased ROM (closer to full knee extension with the hip flexed to 90°) and agrees with the patient’s assessment. “Good work! Your hamstring is less stiff.” And that makes sense. Until you dig deeper and realize that stiffness means something a bit more mathematical in the engineering world. And measuring it in the clinic takes a bit more than what I was measuring with my goniometer.
An engineer or clinician measuring stiffness for research purposes would define the extent to which the tissue resists deformation (change in length) in response to an applied force. And remember that tissue is viscoelastic, so that really gets complicated (at least for my physiology brain). You can imagine my confusion when I walked into my first tissue engineering lab meeting (Ray Vanderby, PhD, one of the best mentors ever) and learned that tendon stiffness was good??? Huh? Hadn’t I been rewarding my compliant patients (no pun intended) for decreasing stiffness through stretching? Yes, stiffness as defined by loss of flexibility is something we want to improve with stretching. Tendon stiffness, as defined by stress / strain and a time dependent modulus thrown in (not what I was measuring in the clinic), allows efficient transfer of force of the muscle to move the limb in cycling and all other forms of movement is something we would like to preserve. As we age, tendon stiffness declines. Think about Tigger at 40. Or 80. Eccentric exercise and plyometrics are ways to improve tissue stiffness. Stretching does not decrease stiffness. At least that’s my understanding.
Chronic stretching with improvement in ROM has been attributed to the myogenic response of sarcomeres adding more functional units in series to lengthen a muscle. Said simply, a muscle shortened due to posture, injury or immobilization is not optimized. Stretching may restore tissue length to decrease strain and optimize the crossbridge interaction of the contractile proteins, myosin and actin, for force development through sarcomerogenesis. A sarcomere is the functional unit of muscle, and genesis indicates the addition of sacromeres in series to restore length. This may be particularly important following muscle injury or immobilization.
Does stretching prevent injury? Several prospective studies have failed to show an effect of stretching on injury rates. However, lack of flexibility may impact joint health by limiting ROM and therefore synovial fluid bathing of the cartilage (remember the Tin Man?), creating abnormal stress on adjacent joints, and is a risk factor for strain induced muscle damage.
If you subscribe to stretching as part of your quest to maintain or increase flexibility, how do you best go about it? There are many types of stretching, and the nomenclature can be confusing. Similar to the zone model of aerobic training, there is no agreement on one set of terms to describe stretching. For the purposes of this article, we will define stretching modes as passive or active, referring to the state of muscle contraction. The term dynamic warmup was introduced earlier to describe exercises for mobility, and therefore won’t be used to describe flexibility training.
Passive stretching implies to lengthening of the muscle, tendon and fascia without contraction. This is the most traditional form of stretching that many of us were introduced to in physical education.
Passive calf stretch, with static hold for 15-30 seconds, 2-4 repetitions.
The data suggests that passive stretching improves ROM, likely through stretch tolerance rather than tissue length, and reduces muscle soreness when performed after an exercise session. Cautionary note: most of the detrimental effects of stretching on muscle strength and performance are attributed to the static mode of stretching prior to exercise. From a physical therapy perspective, static stretching is valuable for patients recovering from muscle injury or immobilization following surgery.
Active stretching, in this context, refers to a contraction of a muscle just prior to stretching. This concept is rooted in work done by physician Dr. Herman Kabat and physical therapist Margaret Knott between 1946- 1954 called proprioceptive neuromuscular facilitation (PNF). Briefly, proprioceptors are sensors that detect changes in body position or movement. Specifically, muscle spindles and Golgi tendon organs (GTO) report changes in length and rate of stretch from within muscle or tendon, respectively, and convey these to the central nervous system. It is beyond the scope of this article (and my ability) to describe the physiology more completely. It has been suggested that there is a neurological effect, evidenced by increase in ROM in the non-PNF stretched limb due in part to proprioceptors causing autogenic and reciprocal inhibition. Stately simply, the core principle of PNF is that a muscle contraction will facilitate relaxation.
Hold-Relax (HR) and Contract-Relax (CR) are PNF techniques whereby firing the target muscle (TM) causes GTO excitation. Following contraction, there is a refractory period, termed autogenic inhibition, allowing enhanced lengthening. Similarly, with Contract-Relax Agonist Contraction (CRAC), contraction of the muscle opposite the TM (i.e., contracting the hamstrings while stretching the quadriceps) will excite the muscle spindles, causing reciprocal inhibition of the TM (the body is not wired to have antagonistic muscles firing at the same time- it would be difficult to move), facilitating stretch. Whatever the mechanism, active PNF stretching has been demonstrated (not unequivocally) to be more effective than static stretching for increasing ROM.
Anecdotally, speaking from 30 years of experience working with athletes, PNF is my go-to. Here are two examples of how to incorporate PNF techniques. Note: there are various definitions and prescriptions for HR, CR, and CRAC. The following examples may take liberties from the official PNF literature.
Hold-Relax or Contract-Relax for Hamstrings: athlete uses a strap to passively extend the lower leg until tension is felt in the hamstrings. Athlete then performs ~70% maximal hamstring contraction with no (HR) or little movement (CR) for ~10 seconds. Upon relaxation, the strap is used to further stretch the hamstring ~20 seconds. HR/CR is repeated 2-3 times.
Contract-Relax Agonist Contraction for Quadriceps: athlete holds ankle of target leg to prevent movement, and performs an isometric contraction of quadriceps muscle at or above 70% max for ~10 seconds. Upon relaxation, athlete maximally fires the hamstrings for ~5 seconds as the knee is pulled into greater flexion and held for ~20 seconds. CRAC is repeated 2-3 times.
You may be wondering where yoga falls into the realm of flexibility. Yoga is much more than flexibility training: it includes stability, balance and community. A humbling moment for me was taking my first yoga class a few years ago, and realizing that the instructor (and dear friend) knew more about stretching than I did a physical therapist and muscle physiologist. Fascia doesn’t run in a single plane. So why had I been instructing patients and athletes to stretch muscles in a single plane??? Some cyclists happily incorporate yoga into their rest and recovery day, while others balk at the idea of spending an hour exploring Warrior poses. I would encourage you to check out a class and decide for yourself (see the community partner page on my website). She has created two short 20 minute “essentials” yoga video targeting muscle groups most often plagued by repetitive motions of cycling available to those who Draft Responsibly.
Hierarchy of Movement: Mobility
It all begins with an idea.
January 2025
Welcome to the second installment of the newsletter. Last month, we identified demands in cycling that lead to common musculoskeletal impairments, and outlined how to triage these impairments. The new year offers a great opportunity to establish a routine to help mitigate these impairments. The aim of this newsletter is to provide a basic framework for adding tools to your toolbox to build a more plastic, resilient, durable cyclist.
We are all familiar, and some obsessed, with the mechanics of pedaling a bicycle. And while we have come to love the predictability of pedaling repetitively in one plane of motion (on average 4800 revolutions in one hour), it is easy to lose sight of the foundational movements that brought us to ride our glorious steeds. The hierarchy of movement is built on mobility, flexibility, stability, strength and skill/ functional proficiency. The off-season is a time to redirect efforts away from the apex (skill/functional proficiency) and back to basics, rebuilding weak spots in the foundation, starting with mobility. Future newsletters will address flexibility, stability and strength.
Mobility is described by the “3 Fs” (by me and nobody else, so don’t bother Googling 3-Fs as it may indeed take you down a dark path, requiring you to clear your search history): control of movement freely and fluidly through a functional range of motion (ROM). The best illustration of this is to watch an infant as they gain control over their arms and hands, moving freely and fluidly through a functional ROM to suck their thumb. The infant lacks sufficient stability to hold an object of appreciable mass, strength to launch it, skill to aim it, but is mastering mobility. Aging and injuries can hinder mobility by changing the articulating surfaces of joints. Synovial fluid, nature’s WD40 for joints, decreases with age (think about the Tin Man in the Wizard of Oz to help visualize the effect of aging and injury on mobility), making us feel a bit creaky.
The key to maintaining mobility is to ensure each link in the kinetic chain is functional, starting with the foot- ankle complex and working up through the cervical spine. Cyclists are often aware when they lack mobility in the sagittal plane at the hip or knee, as it becomes difficult to pedal, but often ignore loss of mobility in other planes and other joints. Loss of mobility at one segment can affect the structure and function of the segments above and below, greatly altering their ability to function. For example, cyclists often neglect ankle mobility, given the non-impact nature of the sport. Limited mobility at the ankle joint requires greater mobility at the knee or hip joint in order for the kinetic chain to complete the pedal stroke. Excessive or aberrant motions cause unwarranted stress at these more proximal joints, increasing the potential for injury.
Mobility exercises can be easily incorporated into a dynamic warmup routine prior to aerobic or strength training. Deep squats with arms overhead, hurdle step-over and back, lateral hurdle step-over and step-under, lunges in 3 directions (forward, backward and lateral) with arms overhead are lower extremity mobility exercises. The master of mobility (and all things movement related), Steve Myrland, has shared some videos called “Happy Hips and Hamstrings” and Strength and Length with Jungle Gym that are extremely helpful. Upper extremity mobility exercises can be facilitated with a dowel, PVC tubing, broom or other stick like device that can be held at arm’s length. Steve has dubbed one such exercise “hayforks”; starting in a staggered stance, using the stick (pitchfork) for the lower arm to drive the upper arm overhead, alternating sides. Windmills, side lean and lengthen can also be facilitated with the dowel. More aggressive mobility exercises include skipping forwards, backwards and laterally and leg swing heel touches with opposite arm. As tissue temperature increases, these movements progress with increased ROM and speed through successive repetitive motions until end of the range is achieved.
In order to execute the more aggressive mobility exercises safely, adequate flexibility is required. Flexibility is defined as ability of muscle, tendon and fascia to lengthen passively (in the absence of muscle contraction) through ROM. Flexibility training will be the topic of the next newsletter.
Common Impairments in the Cyclist
Common impairments in the cyclist.
December 2024
December. It is hard to know what the season will bring. Last Saturday was Global Fat Bike Day, hinting at winter fun in the snow, and Sunday was near 50°, begging for pedaling road bikes. Regardless of the temperature, winter for the cyclist should be restorative. For those with a penchant for pedaling, dismounting our trusty steads in the off-season may prove more challenging than committing to grueling miles in-season. Cycling can be a critical component of our physical, social and mental well-being. With time being a limited resource, swapping time on the bike for exercise off the bike can be something we resist, or even fear. Understanding that a movement literacy program isn’t stealing time from the bike, but rather improving and extending the ride, can allay those fears. Don’t worry about sounding professional. Sound like you. There are over 1.5 billion websites out there, but your story is what’s going to separate this one from the rest. If you read the words back and don’t hear your own voice in your head, that’s a good sign you still have more work to do.
Building a strong cyclist is relatively straight forward: pedal harder, pedal faster, pedal further, rest and repeat. Building a plastic, resilient and durable cyclist is more complicated and requires more tools in the training toolbox. This newsletter hopes to 1) identify demands in cycling that lead to common musculoskeletal impairments, 2) outline how to triage these impairments. Subsequent newsletters will provide a basic framework for a movement literacy training program to mitigate these impairments and complaints.
Many cyclists find the act of pedaling to be second nature. However, cycling is not a natural part of human movement. While humans have been ambulating upright for nearly 6 million years, movement via bicycle was only recently introduced (roughly 200 years ago). Bodies are not optimized for repetitive motion of the lower extremities with near maximal hip flexion, confined to a single plane with several fixed contact points. Pedaling a bicycle demands opposing muscles in the sagittal plane to be chronically positioned in shortened and lengthened positions, respectively. This posture has a propensity to create musculoskeletal imbalances that can be described as cross-over syndrome. In addition, the lack of impact loading and eccentric contractions can diminish bone health and the tensile strength of tendons.
Cross-over syndrome of the upper extremities is characterized by tightness through the pectoral muscles of the chest, upper trapezius and sub-occipital muscles at the base of the skull. The opposing muscles, namely the middle and lower trapezius and deep neck flexors, may develop weakness as they are chronically held in a sub-optimal lengthened position (stretch weakness). These muscle imbalances are exemplified by a forward head and thoracic kyphotic posture. Cyclists may experience a myriad of symptoms secondary to this postural dysfunction, including neck and shoulder pain. In the lower extremities, the imbalance creates tightness through the hip flexors and low back extensors, which act on the pelvis. The gluteal and abdominal muscles, placed in a non-optimal stretch position, struggle to counter the forces on the tight muscles on the pelvis. The resulting posture is one of increased anterior pelvic tilt and hyper-lordosis. This places ligamentous strain on the lower lumbar vertebrae and sacroiliac joints. Due to the nature of the human kinetic chain, dysfunction at one segment, in this case the lumbo-pelvic segment, frequently leads to dysfunction at adjacent and distal segments, including the hip and knee. Furthermore, cycling is a quadriceps dominated activity. Ensuring the proper hamstring to quadriceps strength ratio is critical for knee stability for sports outside of cycling.
The foot- ankle complex is another region that may suffer cycling. The foot- ankle complex is designed to undergo both supination (plantarflexion, adduction and inversion) and pronation (dorsiflexion, abduction and eversion) during push off and mid-stance phases of gait, respectively. This allows the foot to be locked in a rigid and stable position during push off and unlocked to accommodate ground reaction forces during midstance. The biphasic nature of motion is lost during cycling, with the majority of time spent in the unlocked position of pronation, which may lead to strain on the arch and compression of the neurovascular structures (hot foot).
The cyclist is not doomed for discomfort, but it does take a concerted effort to build a plastic, resilient and durable cyclist that requires tools in the training toolbox beyond pedaling. These tools are part of what is referred to as movement literacy, built on a hierarchy of mobility, flexibility, stability, strength and skill/ functional proficiency. Armed with these tools, musculoskeletal impairments that hinder movement patterns on and off the bike may be mitigated. Finding the right “technician” with mastery of the tools to work on your “machine” can be a daunting task. Many cyclists take the “whack-a-mole approach”. Desperate to be back in the saddle pain free, they engage practitioners across a variety of disciples to render aid. While this approach is rarely dangerous and may ultimately result in resolution of symptoms, collateral damage may occur to your pocket book and delay effective treatment. Time is a precious resource, so why squander it? A silly but relevant analogy is triaging a poorly running vehicle. Desperate to get the car running smoothly, you may solicit a several service technicians who replace the battery, fuel line and alternator before running a diagnostic test, only to learn the problem is a faulty spark plug. No damage was done to the vehicle (in fact, it has lots of new parts that didn’t need replacing), but precious time and money were used treating symptoms rather than identifying the underlying cause. The best place to start when your body isn’t running smoothly is with a proper diagnosis.
If the tools in your toolbox (stretching, yoga, strengthening) aren’t moving the needle, and symptoms have persisted for more than 6 weeks with rest, it would be prudent to investigate the source, rather than continue to treat the symptoms. A physician or physical therapist trained in sports medicine is a good starting point. A physician may order diagnostic tests, such as a radiograph or MRI. While not every musculoskeletal injury requires diagnostic imaging, identify the underlying etiology of the impairment or compliant is paramount to providing effective treatment. While rare, in my role as a physical therapist treating cyclists, I have come across lateral knee pain caused by an osteosarcoma masquerading as iliotibial band syndrome and recalcitrant back pain caused by a tumor. The whack-a-mole approach would have not have served these athletes well. More commonly, cyclists are plagued by overuse musculoskeletal issues such as tendinopathy, patellofemoral stress syndrome, low back, neck and shoulder pain whereby imaging may be ordered to confirm the diagnosis and inform the conservative treatment. These pathologies are often best addressed by a physical therapist with working knowledge of cycling demands and bicycle fit.
Solving biomechanical puzzles can be complicated as cycling involves two machines: one with two legs interfacing with another with two wheels. There are very few other sports whereby the solution may lie with either or both machines. Here is a case scenario to illustrate the point: a cyclist with 20 years of experience presents with a gradual onset of knee pain at the end of his cycling season in October, without changes in training volume or injury. His coach recommends the athlete be seen by a physical therapist. Evaluation reveals lack of hamstring and iliotibial band flexibility with poor gluteal firing, leading to patellofemoral stress syndrome (PFSS). These findings could certainly predispose the athlete to PFSS, but there is little in his history to suggest that these impairments alone, likely present for many years, are the only precipitating factors in developing knee pain late in the season. Further evaluation of his equipment reveals worn cleats and the cyclist recalls a recent adjustment after the saddle became loose, inadvertently resulting with nose down 5°. A myriad of factors contributed to the onset of knee pain, and only careful evaluation of the body and bike together allowed full resolution. Once the underlying factors had been identified, skilled technicians with the appropriate tools were employed. His PT prescribed exercises to address the impairments, a bike mechanic replaced the cleats, readjusted the saddle position and educated the client on how to tighten the saddle without creating tilt, and the client asked his massage therapist to focus the session on his IT band. There is a wide variety of practitioners with similar tools: chiropractors, physical therapists, massage therapists, strength and conditioning coaches, personal trainers. Nobody has every tool in their box. Some offer many tools with little experience using them, while others have only a few tools but have mastered their craft. The best technicians are those who know what they don’t know, and have created a network of technicians to collectively offer the largest tool box for the athlete.
The next newsletter will provide a basic framework for adding tools to your toolbox to build a more plastic, resilient, durable cyclist.